Specific Abnormalities
Abnormal scan results? We make sure you are fully informed
Nobody wants to be told they have a heart condition; we believe a more complete understanding empowers you to take the next steps.
Understanding your results in detail.
Echo scans are reported according to internationally established guidelines. As a consequence, the scan results contain numerous technical terms, figures and calculations, which can be readily interpreted by Heart Specialists all over the world, but can be confusing for the non-expert. An explanation of the key anatomical terms and scan findings follows below.
If you need further information on specific cardiac abnormalities, you can find it here.
Search for answers here:
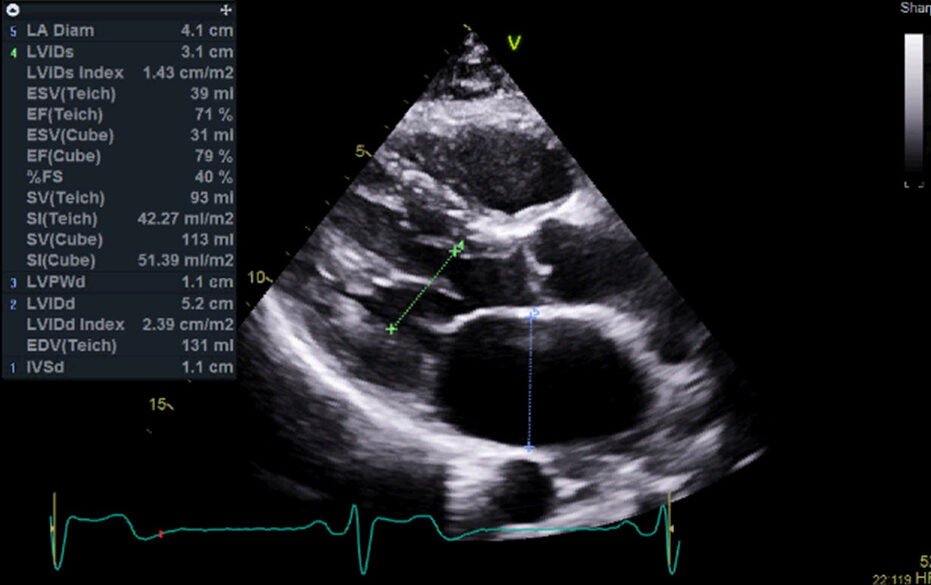
Chamber size is a critical aspect of heart health that plays a significant role in the heart's ability to function effectively. The heart is composed of four chambers - two atria (upper chambers) and two ventricles (lower chambers) - each of which must maintain an optimal size for efficient blood circulation. Abnormalities in chamber size, whether an enlargement or a reduction, can indicate underlying heart conditions and may lead to serious health complications if left unaddressed.
This page covers everything you need to know about chamber size, including its definition, the seriousness of abnormal chamber sizes, types of conditions associated with chamber size changes, symptoms, causes, available treatments, the role of heart scans in diagnosis, and the importance of trusting a professional cardiac clinic for management and care.
Defining Chamber Size
The size of the heart chambers is crucial for the effective pumping of blood. The atria receive blood from the body and lungs, while the ventricles pump blood to the lungs and the rest of the body. Under normal conditions, each chamber maintains a specific size that ensures efficient blood flow through the heart and to the rest of the body.
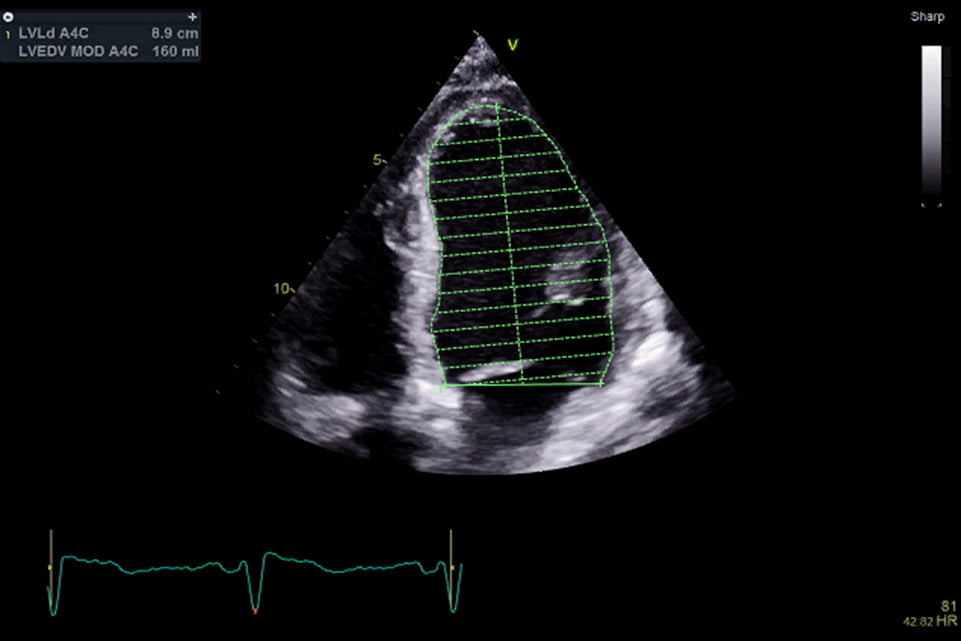
The dimensions of the heart chambers can be measured using imaging techniques such as echocardiography, and these measurements are critical for assessing heart health. The size of the chambers can be influenced by various factors, including age, body size, and physical conditioning. However, significant deviations from normal chamber size can be a sign of pathological conditions that require medical attention.
How Serious Is It? & Are There Different Types?
Abnormal chamber sizes can be a serious health concern, depending on the extent and nature of the changes. The seriousness often correlates with the underlying cause and the specific chamber(s) involved.
- Atrial Enlargement: Enlargement of one or both atria is often associated with conditions such as atrial fibrillation, hypertension, and valvular heart disease. Atrial enlargement can lead to inefficient blood flow and an increased risk of blood clots, which can cause strokes.
- Ventricular Enlargement (Cardiomegaly): Ventricular enlargement, particularly of the left ventricle, is often seen in conditions such as hypertension, cardiomyopathy, and heart failure. This can lead to a reduced ability of the heart to pump blood effectively, potentially leading to congestive heart failure.
- Dilated Cardiomyopathy: A condition where the heart chambers enlarge and the heart muscle becomes weak, leading to reduced pumping ability and heart failure. This is a severe condition that requires ongoing management.
- Ventricular Hypertrophy: This involves the thickening of the ventricular walls, often due to increased workload on the heart from conditions like hypertension. While the walls thicken, the chamber size may reduce, leading to decreased blood volume in each heartbeat, which can be dangerous if untreated.
Symptoms
The symptoms associated with abnormal chamber size can vary widely depending on the underlying condition and severity:
- Shortness of breath: This is a common symptom as the heart struggles to pump blood efficiently, leading to fluid buildup in the lungs.
- Fatigue: Due to the reduced efficiency of blood circulation, patients often feel tired and lack energy.
- Palpitations: Irregular or rapid heartbeats may occur, particularly in cases of atrial enlargement.
- Chest pain or discomfort: This can result from the heart working harder to pump blood, especially in conditions like ventricular hypertrophy.
- Swelling (edema): Particularly in the legs, ankles, and feet, due to poor blood circulation.
- Fainting (syncope): In severe cases, poor blood flow can lead to dizziness or fainting.
Causes
Several factors can cause abnormal chamber sizes:
- Hypertension: Chronic high blood pressure forces the heart to work harder, leading to enlargement, particularly of the left ventricle.
- Heart valve disease: Conditions like mitral valve regurgitation or aortic stenosis can cause the chambers to enlarge as the heart compensates for the faulty valve.
- Coronary artery disease: Reduced blood flow to the heart muscle can weaken it, leading to chamber enlargement.
- Cardiomyopathy: Diseases of the heart muscle can lead to changes in chamber size, often resulting in either dilated or hypertrophic cardiomyopathy.
- Congenital heart defects: Some people are born with structural heart abnormalities that can affect chamber size.
- Chronic lung disease: Conditions like chronic obstructive pulmonary disease (COPD) can lead to right ventricular enlargement due to increased pressure in the pulmonary arteries.
Available Treatments
Treatment for abnormal chamber size depends on the underlying cause and severity:
- Medications: Drugs such as ACE inhibitors, beta-blockers, and diuretics can help manage the symptoms and reduce the heart's workload, slowing the progression of chamber enlargement.
- Lifestyle changes: Managing contributing factors like hypertension through diet, exercise, and weight loss is essential.
- Surgical intervention: In severe cases, surgery may be required to repair or replace damaged heart valves or to correct congenital defects.
- Implantable devices: Pacemakers or defibrillators may be necessary to manage heart rhythm problems associated with chamber enlargement.
The Role of Heart Scans in Identifying The Issue
Heart scans are essential for diagnosing abnormal chamber sizes and determining the severity of the condition. The most common imaging tests include:
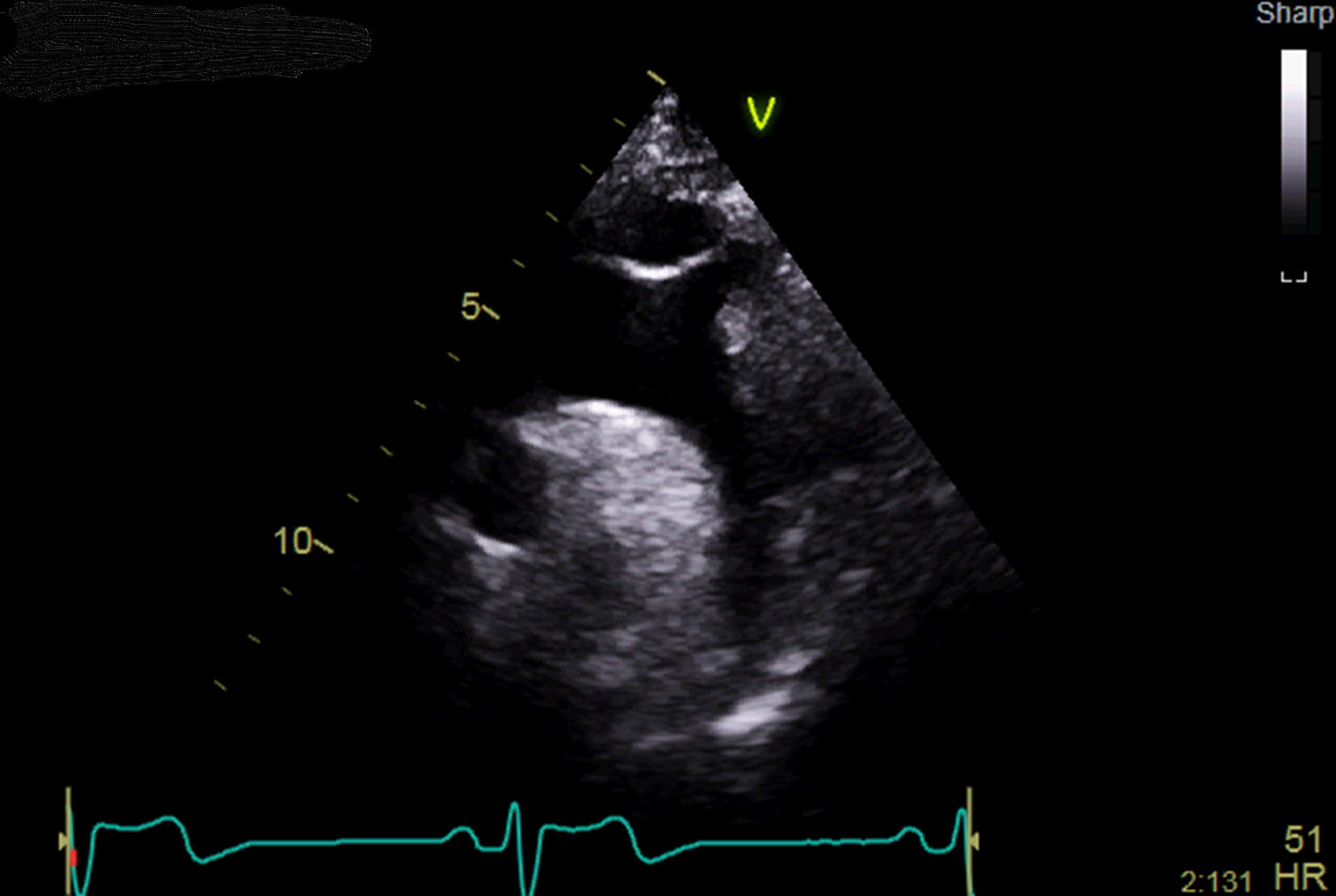
- Echocardiography: This ultrasound-based test is the primary tool for measuring chamber size, providing detailed images of the heart's structure and function.
- Cardiac MRI: Offers a more detailed view of the heart’s anatomy, useful in complex cases or when echocardiography results are inconclusive.
- CT scan: Provides high-resolution images of the heart and is useful in assessing structural abnormalities.
- Chest X-ray: Can show general heart size and detect gross enlargement of the heart chambers.
The Importance of Trusting a Professional Cardiac Clinic
Given the complexity and potential seriousness of issues related to chamber size, it is crucial to seek care from a professional cardiac clinic with experienced cardiologists and access to advanced diagnostic tools.
A specialised cardiac clinic can provide accurate diagnoses, develop personalised treatment plans, and offer ongoing care to manage the condition effectively. Trusting a professional cardiac clinic ensures that patients receive the highest standard of care, which is vital for preventing complications, improving symptoms, and enhancing long-term outcomes.
In conclusion, chamber size is a fundamental aspect of heart health that requires careful monitoring and management when abnormalities are detected. Understanding the symptoms, causes, and treatment options, along with the importance of professional care, is essential for maintaining heart health and overall well-being.
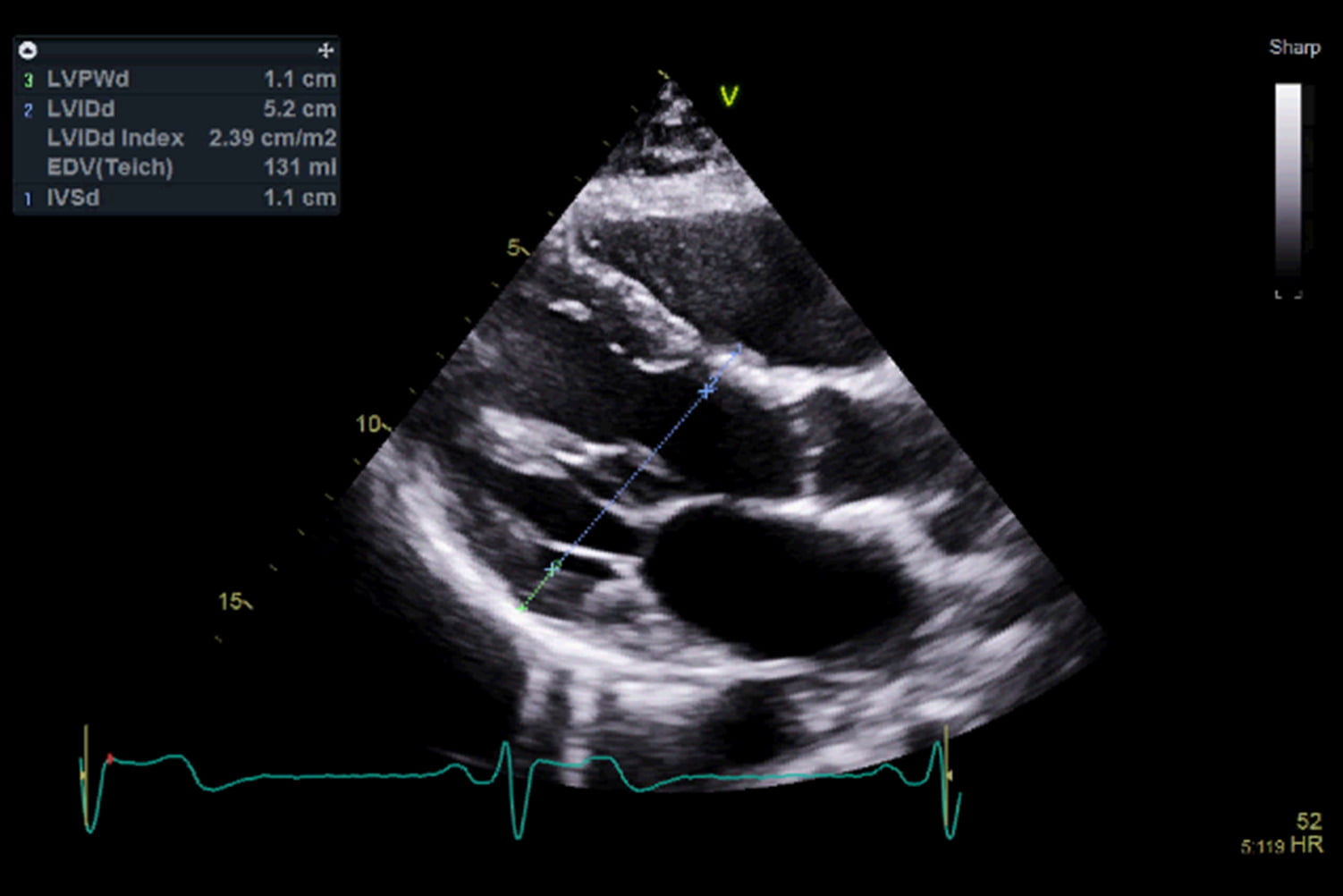
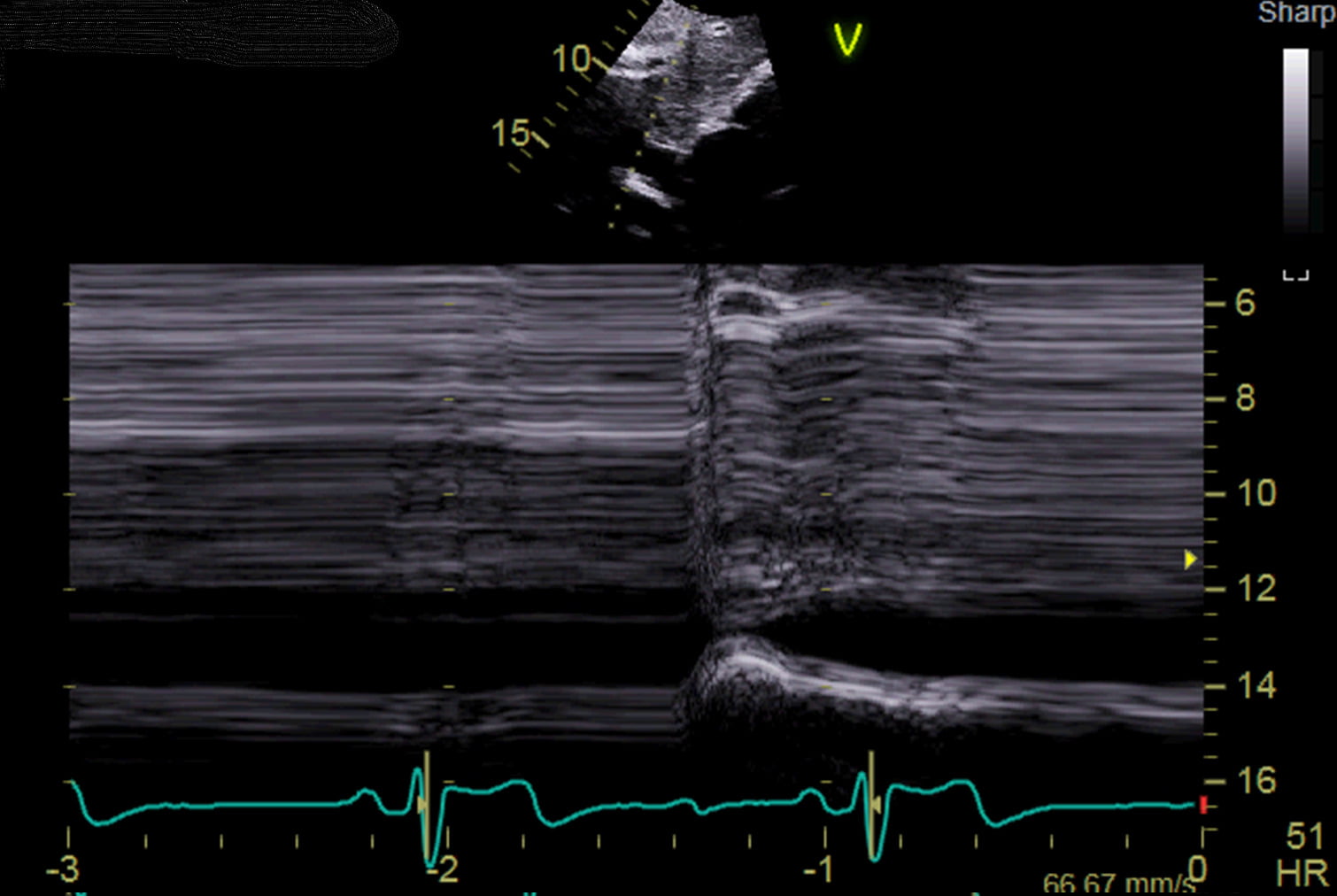
Ventricular wall thickness refers to the measurement of the thickness of the myocardium, which is the muscular wall of the heart's ventricles. The myocardium is responsible for the contractile force that pumps blood out of the ventricles into the pulmonary artery (right ventricle) and aorta (left ventricle).
In a healthy heart, the walls of the ventricles maintain a specific thickness, allowing them to function efficiently. Typically, the left ventricular wall is thicker than the right because it has to pump blood throughout the entire body, whereas the right ventricle only pumps blood to the lungs.
Normal left ventricular wall thickness ranges from 6 to 11 millimetres, while the right ventricular wall is thinner, usually around 3 to 4 millimetres. However, when the ventricular walls become abnormally thick or thin, it can indicate various cardiac conditions, ranging from hypertension-induced hypertrophy to cardiomyopathies.
How Serious Is It? & Are There Different Types?
Changes in ventricular wall thickness can be a serious concern, depending on whether the walls are too thick (hypertrophy) or too thin (atrophy). These changes can affect the heart’s ability to pump blood effectively and may lead to various forms of heart failure or other cardiac complications.
- Left Ventricular Hypertrophy (LVH): This condition is characterised by the thickening of the left ventricular wall. It often occurs in response to increased workload on the heart, such as from high blood pressure (hypertension) or aortic valve stenosis. While initially a compensatory mechanism, LVH can lead to stiffening of the heart muscle, reduced blood flow, arrhythmias, and heart failure if left untreated.
- Right Ventricular Hypertrophy (RVH): The thickening of the right ventricular wall usually results from conditions that increase resistance in the pulmonary circulation, such as chronic lung disease or pulmonary hypertension. RVH can impair the right ventricle’s ability to pump blood efficiently to the lungs, leading to right-sided heart failure.
- Cardiomyopathy: This is a group of diseases that directly affect the heart muscle, leading to changes in ventricular wall thickness. Hypertrophic cardiomyopathy (HCM) is a genetic condition characterised by abnormal thickening of the heart muscle, particularly the septum (the wall between the two ventricles), which can obstruct blood flow and lead to sudden cardiac arrest. Conversely, dilated cardiomyopathy involves thinning of the ventricular walls, resulting in weakened heart contractions and heart failure.
- Ventricular Atrophy: A reduction in ventricular wall thickness, often associated with conditions such as dilated cardiomyopathy, where the heart chambers enlarge and the walls become thin, leading to poor cardiac output.
Symptoms
The symptoms associated with abnormal ventricular wall thickness can vary depending on the underlying condition and severity:
- Shortness of breath: A common symptom, especially during physical activity, as the heart struggles to pump blood effectively.
- Chest pain or discomfort: Particularly with hypertrophic cardiomyopathy, where thickened heart muscle can obstruct blood flow.
- Palpitations: Irregular or rapid heartbeats, often due to arrhythmias associated with hypertrophy.
- Fatigue: Due to reduced cardiac output, leading to inadequate blood supply to the body.
- Dizziness or fainting (syncope): Particularly in cases of hypertrophic cardiomyopathy, where the heart's thickened muscle can obstruct blood flow.
Causes
Several factors can contribute to abnormal ventricular wall thickness:
- Hypertension: Chronic high blood pressure is a leading cause of left ventricular hypertrophy, as the heart must work harder to pump blood against the increased resistance in the arteries.
- Valvular heart disease: Conditions like aortic stenosis, where the aortic valve is narrowed, can cause left ventricular hypertrophy due to the increased effort required to pump blood through the narrowed valve.
- Genetics: Conditions like hypertrophic cardiomyopathy are often inherited and involve mutations that affect the heart muscle's structure and function.
- Chronic lung disease: Conditions like chronic obstructive pulmonary disease (COPD) or pulmonary hypertension can lead to right ventricular hypertrophy due to increased resistance in the pulmonary circulation.
- Athletic training: In some athletes, intense and prolonged physical training can lead to physiological (non-pathological) hypertrophy, where the heart muscle thickens but remains healthy and functional.
Available Treatments
Treatment for abnormal ventricular wall thickness depends on the underlying cause and severity:
- Medications: Drugs such as beta-blockers, ACE inhibitors, or calcium channel blockers may be prescribed to reduce blood pressure, manage symptoms, and improve heart function.
- Lifestyle changes: Managing hypertension through diet, exercise, and weight control is crucial in preventing or reducing ventricular hypertrophy.
- Surgical interventions: In severe cases of hypertrophic cardiomyopathy, surgical procedures like septal myectomy or alcohol septal ablation may be required to reduce the thickness of the heart muscle and improve blood flow.
- Implantable devices: In patients with a significant risk of arrhythmias or sudden cardiac arrest, an implantable cardioverter-defibrillator (ICD) may be recommended.
The Role of Heart Scans in Identifying The Issue
Heart scans play a crucial role in diagnosing changes in ventricular wall thickness and understanding the severity of the condition. Common imaging tests include:
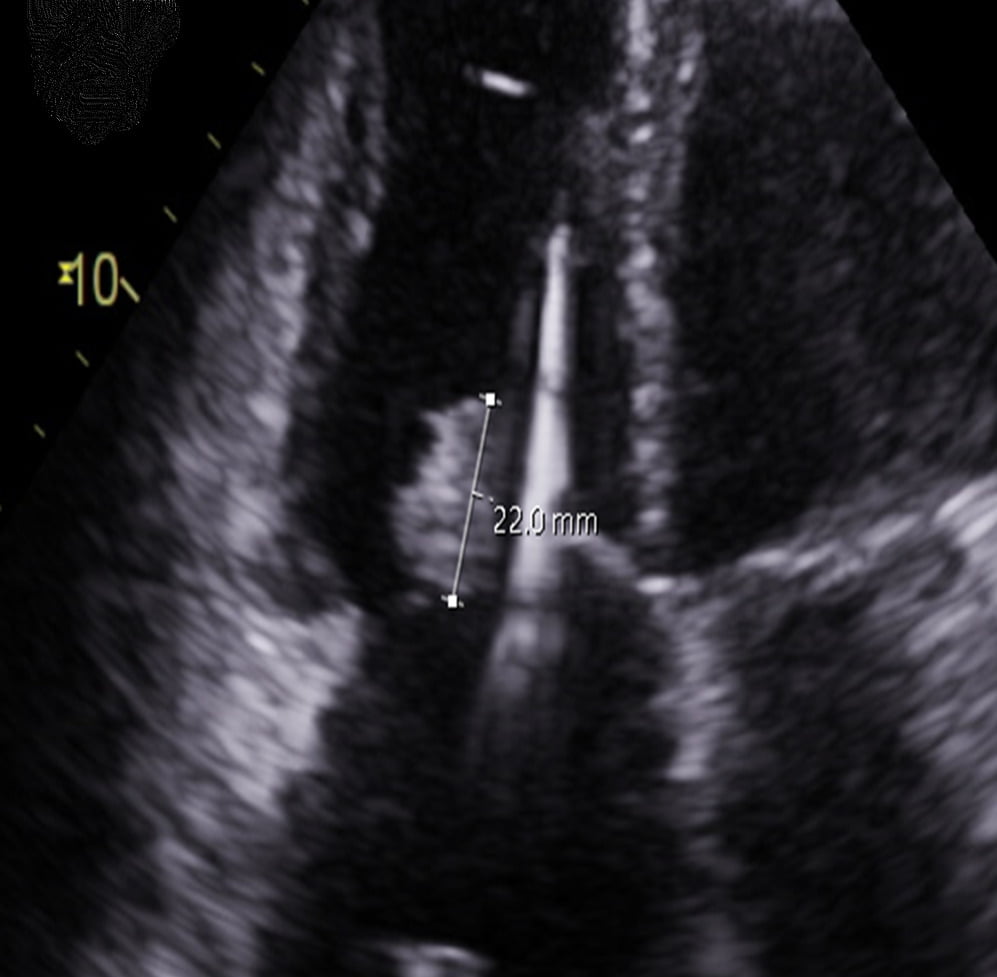
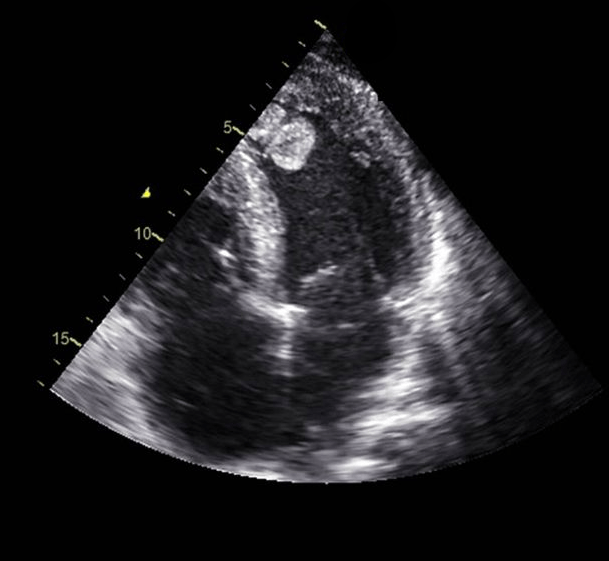
- Echocardiogram: This ultrasound test is the primary tool for assessing ventricular wall thickness, allowing visualisation of the heart's structure and function in real time.
- Cardiac MRI: Provides detailed images of the heart's anatomy, offering precise measurements of wall thickness and muscle mass, which is particularly useful in diagnosing conditions like hypertrophic cardiomyopathy.
- CT scan: Used to assess the heart's anatomy and detect structural abnormalities that may contribute to changes in wall thickness.
- Electrocardiogram (ECG): While not an imaging test, an ECG can detect electrical changes in the heart that may suggest hypertrophy or other related conditions.
The Importance of Trusting a Professional Cardiac Clinic
Given the complexity and potential seriousness of issues related to ventricular wall thickness, it is essential to seek care from a professional cardiac clinic with experienced cardiologists and access to advanced diagnostic tools. A specialised cardiac clinic can provide accurate diagnoses, develop personalised treatment plans, and offer ongoing care to manage the condition effectively. Trusting a professional cardiac clinic ensures that patients receive the highest standard of care, which is crucial for preventing complications, improving symptoms, and enhancing long-term outcomes.
In conclusion, ventricular wall thickness is a vital indicator of heart health, and any abnormalities should be thoroughly evaluated and managed by professionals. Understanding the symptoms, causes, and treatment options, along with the importance of professional care, is essential for maintaining heart health and overall well-being.
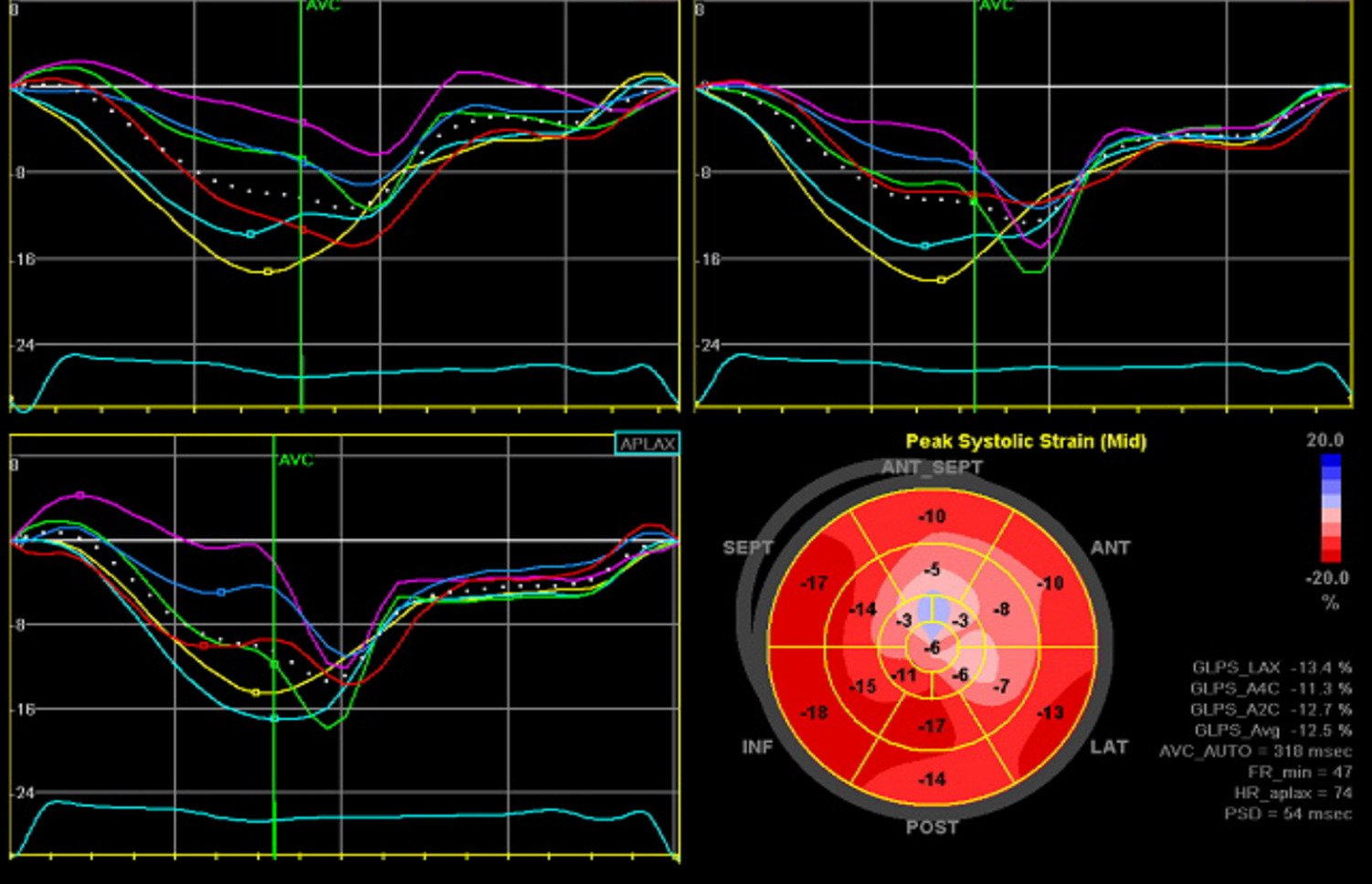
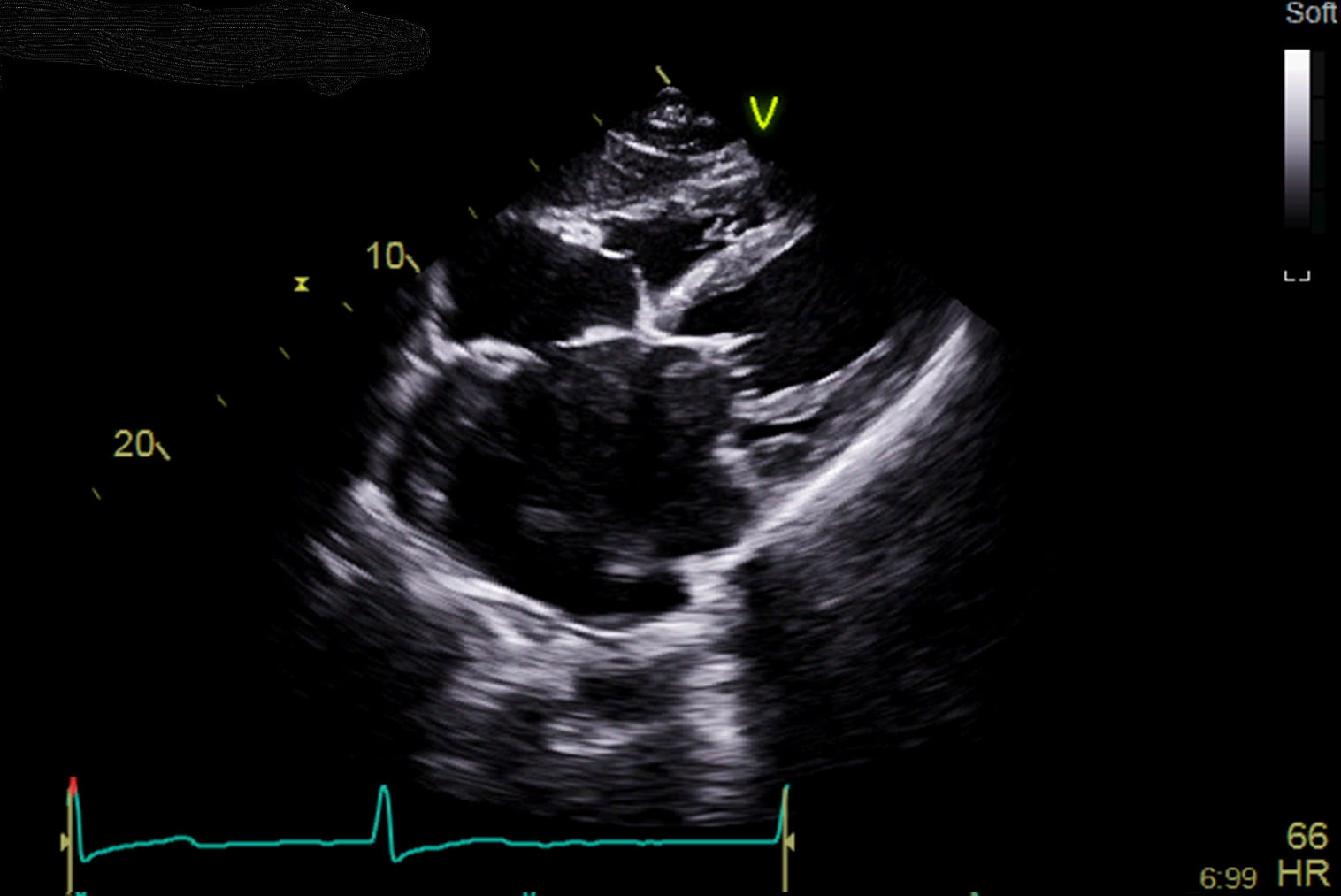
Systolic function refers to the heart’s ability to contract and pump blood out of the ventricles into the arteries, supplying oxygen-rich blood to the body. Healthy systolic function is vital for maintaining adequate blood flow and ensuring that the body's organs and tissues receive the oxygen they need.
This page covers the essential aspects of systolic function, including its definition, the seriousness of impaired systolic function, its types, symptoms, causes, and treatments. Additionally, we explore the role of heart scans in diagnosing systolic dysfunction and emphasise the importance of seeking care from a professional cardiac clinic.
What is Systolic Function?
Systolic function refers to the phase of the cardiac cycle in which the heart's ventricles contract to pump blood out of the heart and into the arteries. During systole, the left ventricle pumps blood into the aorta, which then delivers it to the rest of the body, while the right ventricle pumps blood into the pulmonary artery, sending it to the lungs for oxygenation.
The efficiency of systolic function is critical for maintaining an adequate cardiac output, which is the amount of blood the heart pumps each minute. Systolic function is often assessed by measuring the ejection fraction (EF), which is the percentage of blood ejected from the left ventricle with each heartbeat. A normal ejection fraction typically ranges from 50% to 70%.
How Serious Is It? & Are There Different Types?
Impaired systolic function, also known as systolic dysfunction, is a serious condition that can lead to heart failure and other cardiovascular complications if left untreated. The severity of systolic dysfunction can vary, and it is often classified based on the ejection fraction:
- Mild Systolic Dysfunction: In this stage, the ejection fraction is slightly reduced (40%-49%). The heart's ability to pump blood is mildly impaired, but the patient may not experience significant symptoms.
- Moderate Systolic Dysfunction: The ejection fraction is moderately reduced (30%-39%). The heart's pumping efficiency is significantly impaired, and symptoms such as shortness of breath and fatigue may begin to appear.
- Severe Systolic Dysfunction: The ejection fraction is severely reduced (below 30%). The heart is unable to pump blood effectively, leading to symptoms of heart failure, such as severe shortness of breath, swelling, and exercise intolerance.
Systolic dysfunction can lead to a condition known as heart failure with reduced ejection fraction (HFrEF), where the heart's ability to pump blood is significantly diminished, leading to insufficient blood flow to meet the body's needs.
Symptoms
The symptoms of systolic dysfunction can vary depending on the severity of the condition and may include:
- Shortness of breath: Especially during physical activity or when lying down, as the heart struggles to pump blood efficiently.
- Fatigue: A persistent feeling of tiredness, even with minimal exertion, due to inadequate blood flow to the muscles and tissues.
- Swelling: Particularly in the legs, ankles, and feet, as fluid builds up due to poor circulation and heart failure.
- Chest pain or discomfort: Often due to reduced blood flow to the heart muscle itself.
- Palpitations: Sensations of irregular, rapid, or forceful heartbeats, as the heart tries to compensate for reduced pumping efficiency.
- Exercise intolerance: Difficulty performing physical activities that were previously manageable, often due to reduced cardiac output.
Causes
Systolic dysfunction can result from a variety of underlying conditions or factors:
- Coronary artery disease (CAD): Blockages in the coronary arteries can reduce blood flow to the heart muscle, leading to damage and impaired systolic function.
- Heart attack (myocardial infarction): A heart attack can cause permanent damage to the heart muscle, reducing its ability to contract and pump blood effectively.
- Hypertension: Chronic high blood pressure can strain the heart over time, leading to thickening of the heart muscle (left ventricular hypertrophy) and eventually to systolic dysfunction.
- Cardiomyopathy: Diseases of the heart muscle, such as dilated cardiomyopathy, can weaken the heart's ability to contract, leading to systolic dysfunction.
- Valvular heart disease: Conditions affecting the heart valves, such as aortic stenosis or mitral regurgitation, can increase the workload on the heart and contribute to systolic dysfunction.
- Diabetes: High blood sugar levels can damage the heart muscle and blood vessels, leading to impaired systolic function.
- Obesity: Excess body weight can strain the heart and contribute to the development of systolic dysfunction.
Treatments
Treatment for systolic dysfunction focuses on managing the underlying causes, alleviating symptoms, and improving heart function. Treatment options include:
- Lifestyle changes: Adopting a heart-healthy lifestyle is crucial for managing systolic dysfunction. This includes regular exercise, a balanced diet, weight management, and quitting smoking.
- Medications: Various medications may be prescribed to manage symptoms, reduce the workload on the heart, and improve its function. These may include beta-blockers, ACE inhibitors, angiotensin II receptor blockers (ARBs), diuretics, and aldosterone antagonists.
- Implantable devices: In some cases, devices such as implantable cardioverter-defibrillators (ICDs) or biventricular pacemakers (cardiac resynchronization therapy) may be recommended to help manage heart rhythm and improve systolic function.
- Surgical intervention: For patients with severe systolic dysfunction due to coronary artery disease or valvular heart disease, surgery may be necessary to restore blood flow to the heart muscle or repair/replace damaged heart valves.
The Role of Heart Scans in Identifying The Issue
Heart scans are essential for diagnosing systolic dysfunction and assessing its severity. These imaging tests allow cardiologists to evaluate the heart's structure, measure ejection fraction, and identify any underlying conditions contributing to the dysfunction. Common heart scans used in diagnosing systolic dysfunction include:
- Echocardiogram: An ultrasound of the heart that provides detailed images of the heart's chambers and valves. It is the primary tool for assessing ejection fraction and evaluating systolic function.
- Cardiac MRI: Offers a comprehensive view of the heart's structure and function, including precise measurements of ejection fraction and muscle damage.
- Nuclear Stress Test: Measures how well the heart pumps blood during exercise or stress, helping identify areas of the heart that may not be receiving enough blood.
- Cardiac CT Scan: Provides high-resolution images of the heart's anatomy, helping to identify blockages in the coronary arteries or structural abnormalities that may contribute to systolic dysfunction.
The Importance of Trusting a Professional Cardiac Clinic
Given the complexity and potential seriousness of systolic dysfunction, it is essential to seek care from a professional cardiac clinic with experienced cardiologists and access to advanced diagnostic tools. A specialised cardiac clinic can provide accurate diagnoses, develop personalised treatment plans, and offer ongoing care to manage the condition effectively. Trusting a professional cardiac clinic ensures that patients receive the highest standard of care, which is critical for preventing complications, improving symptoms, and enhancing long-term outcomes.
In conclusion, systolic dysfunction is a significant cardiac condition that requires careful monitoring and appropriate treatment. Understanding its symptoms, causes, and treatment options, along with the importance of professional care, is essential for managing the condition effectively and maintaining a better quality of life.
Diastolic function is a crucial aspect of heart health, as it refers to the ability of the heart's ventricles to relax and fill with blood between contractions. Proper diastolic function is essential for maintaining adequate blood flow throughout the body.
This page explores the concept of diastolic function in detail, including its definition, the seriousness of impaired diastolic function, its types, symptoms, causes, and treatment options. Additionally, we discuss the vital role of heart scans in diagnosing diastolic dysfunction and emphasise the importance of seeking care from a professional cardiac clinic.
What is Diastolic Function?
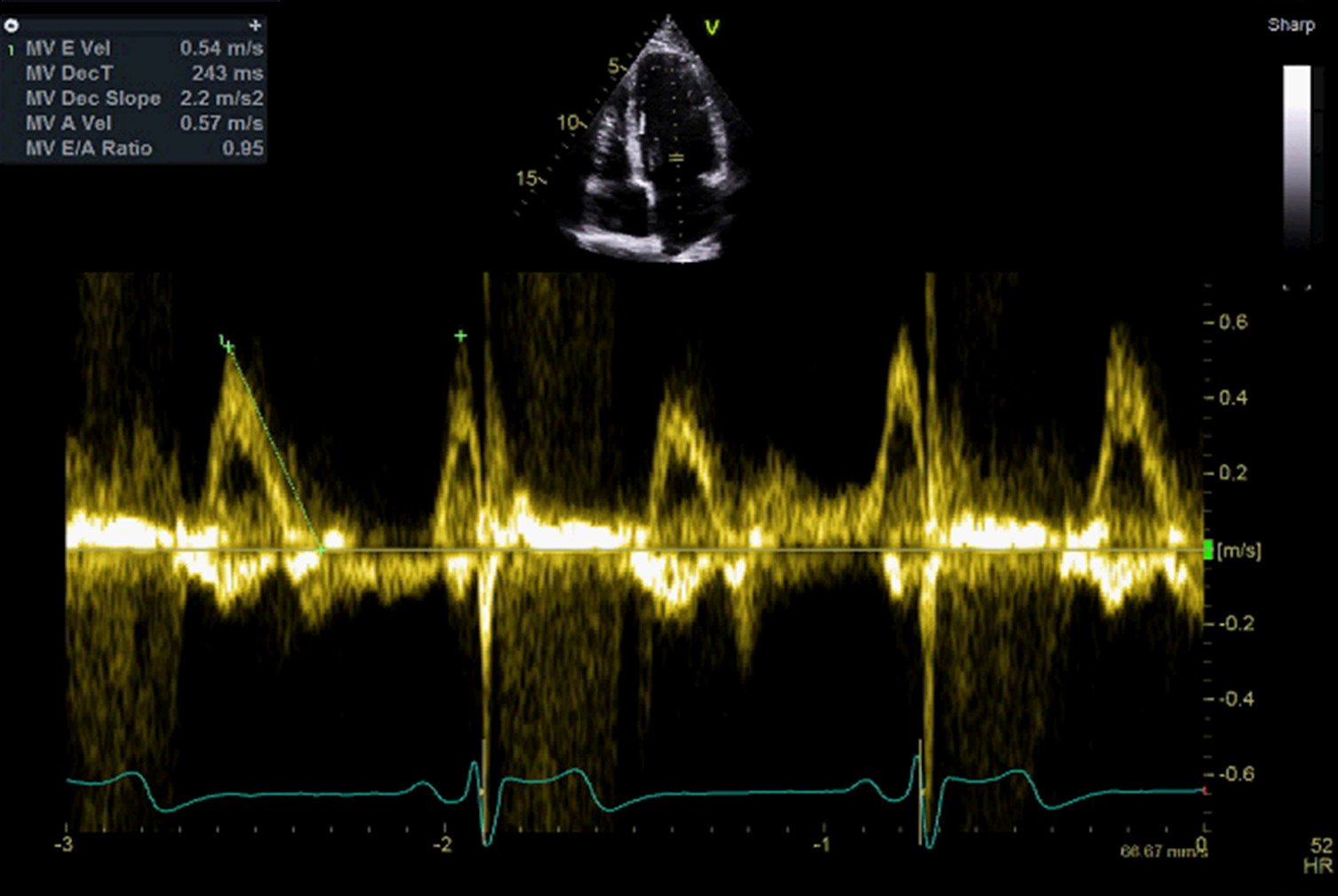
Diastolic function refers to the phase of the cardiac cycle during which the heart's ventricles relax and fill with blood following a contraction (systole). This phase is essential for ensuring that the heart has an adequate volume of blood to pump out to the body during the next contraction.
Diastolic function involves two main processes:
- Ventricular Relaxation: The ability of the ventricles to relax quickly and efficiently after contracting, allowing them to fill with blood.
- Ventricular Filling: The process by which blood flows from the atria into the ventricles during diastole. This filling is influenced by the pressure in the atria and the compliance (flexibility) of the ventricular walls.
Healthy diastolic function is vital for maintaining proper cardiac output and ensuring the body's tissues receive the oxygen-rich blood they need. When diastolic function is impaired, the heart may struggle to fill adequately, leading to multiple health issues.
How Serious Is It? & Are There Different Types?
Impaired diastolic function, also known as diastolic dysfunction, is a serious condition that can lead to heart failure if left untreated. Diastolic dysfunction is typically classified into different grades based on its severity:
- Grade 1 (Mild Diastolic Dysfunction): This is often referred to as "impaired relaxation" and is the earliest stage of diastolic dysfunction. In this stage, the ventricles are slower to relax, but the overall filling is still adequate due to compensatory mechanisms. Many individuals with grade 1 diastolic dysfunction may not experience noticeable symptoms.
- Grade 2 (Moderate Diastolic Dysfunction): Also known as "pseudonormal filling," this stage represents a more advanced level of dysfunction. The ventricles struggle more significantly to relax, and the heart begins to compensate by increasing filling pressures. Symptoms such as shortness of breath and fatigue may start to appear.
- Grade 3 (Severe Diastolic Dysfunction): In this stage, also known as "restrictive filling," the ventricles are stiff and unable to relax properly, leading to significantly impaired filling. This stage is associated with elevated filling pressures and symptoms of heart failure, such as severe shortness of breath, swelling, and exercise intolerance.
Diastolic dysfunction can lead to heart failure with preserved ejection fraction (HFpEF), a condition where the heart's ability to pump blood is normal, but its ability to fill is compromised, leading to insufficient cardiac output.
Symptoms
The symptoms of diastolic dysfunction may vary depending on the severity of the condition and may include:
- Shortness of breath: Especially during physical activity or when lying down.
- Fatigue: A persistent feeling of tiredness, even with minimal exertion.
- Swelling: Particularly in the legs, ankles, and feet, due to fluid buildup.
- Chest discomfort: Although less common, some individuals may experience chest pain or discomfort.
- Palpitations: A sensation of irregular or rapid heartbeats.
- Exercise intolerance: Difficulty performing physical activities that were previously manageable.
Causes
Diastolic dysfunction can result from various factors and underlying conditions:
- Hypertension: Chronic high blood pressure is a leading cause of diastolic dysfunction. Over time, hypertension can cause the ventricular walls to thicken (left ventricular hypertrophy), reducing their ability to relax and fill properly.
- Ageing: As people age, the heart's tissues become stiffer, which can impair diastolic function.
- Coronary artery disease (CAD): Blockages in the coronary arteries can lead to ischemia (reduced blood flow) and damage to the heart muscle, affecting its ability to relax.
- Diabetes: High blood sugar levels can damage the heart's blood vessels and contribute to stiffening of the ventricular walls.
- Obesity: Excess body weight can strain the heart and contribute to the development of diastolic dysfunction.
- Valvular heart disease: Conditions such as aortic stenosis or mitral regurgitation can increase the workload on the heart, leading to diastolic dysfunction.
- Cardiomyopathy: Diseases that affect the heart muscle, such as hypertrophic cardiomyopathy or restrictive cardiomyopathy, can impair diastolic function.
Available Treatments
Treatment for diastolic dysfunction focuses on managing the underlying causes, alleviating symptoms, and preventing the progression to heart failure. Treatment options include:
- Lifestyle changes: Adopting a heart-healthy lifestyle is crucial for managing diastolic dysfunction. This includes regular exercise, a low-sodium diet, weight management, and quitting smoking.
- Medications: Various medications may be prescribed to manage blood pressure, reduce fluid buildup, and improve heart function. These may include diuretics, beta-blockers, calcium channel blockers, and ACE inhibitors.
- Blood pressure control: Maintaining optimal blood pressure is essential for preventing further damage to the heart and improving diastolic function.
- Treating underlying conditions: Managing conditions like diabetes, coronary artery disease, and obesity can help improve diastolic function and reduce symptoms.
- Surgical intervention: In cases where diastolic dysfunction is caused by valvular heart disease, surgery may be necessary to repair or replace the affected valve.
The Role of Heat Scans in Identifying The Issue
Heart scans are critical for diagnosing diastolic dysfunction and assessing its severity. These imaging tests allow cardiologists to evaluate the heart's structure, measure diastolic function, and identify any underlying conditions contributing to the dysfunction. Common heart scans used in diagnosing diastolic dysfunction include:
- Echocardiogram: An ultrasound of the heart that provides detailed images of the heart's chambers and valves. It can measure the rate of ventricular relaxation, assess the size and thickness of the heart chambers, and estimate filling pressures.
- Doppler Echocardiography: A specialised type of echocardiogram that measures blood flow through the heart's chambers, helping to identify abnormalities in diastolic filling.
- Cardiac MRI: Offers a comprehensive view of the heart's structure and function, including detailed measurements of ventricular relaxation and filling.
- Cardiac CT Scan: Provides high-resolution images of the heart's anatomy, helping to identify structural abnormalities that may contribute to diastolic dysfunction.
The Importance of Trusting a Professional Cardiac Clinic
Given the complexity and potential seriousness of diastolic dysfunction, it is essential to seek care from a professional cardiac clinic with experienced cardiologists and access to advanced diagnostic tools. A specialised cardiac clinic can provide accurate diagnoses, develop personalised treatment plans, and offer ongoing care to manage the condition effectively. Trusting a professional cardiac clinic ensures that patients receive the highest standard of care, which is critical for preventing complications, improving symptoms, and enhancing long-term outcomes.
In conclusion, diastolic dysfunction is a significant cardiac condition that requires careful monitoring and appropriate treatment. Understanding its symptoms, causes, and treatment options, along with the importance of professional care, is essential for managing the condition effectively and maintaining a better quality of life.
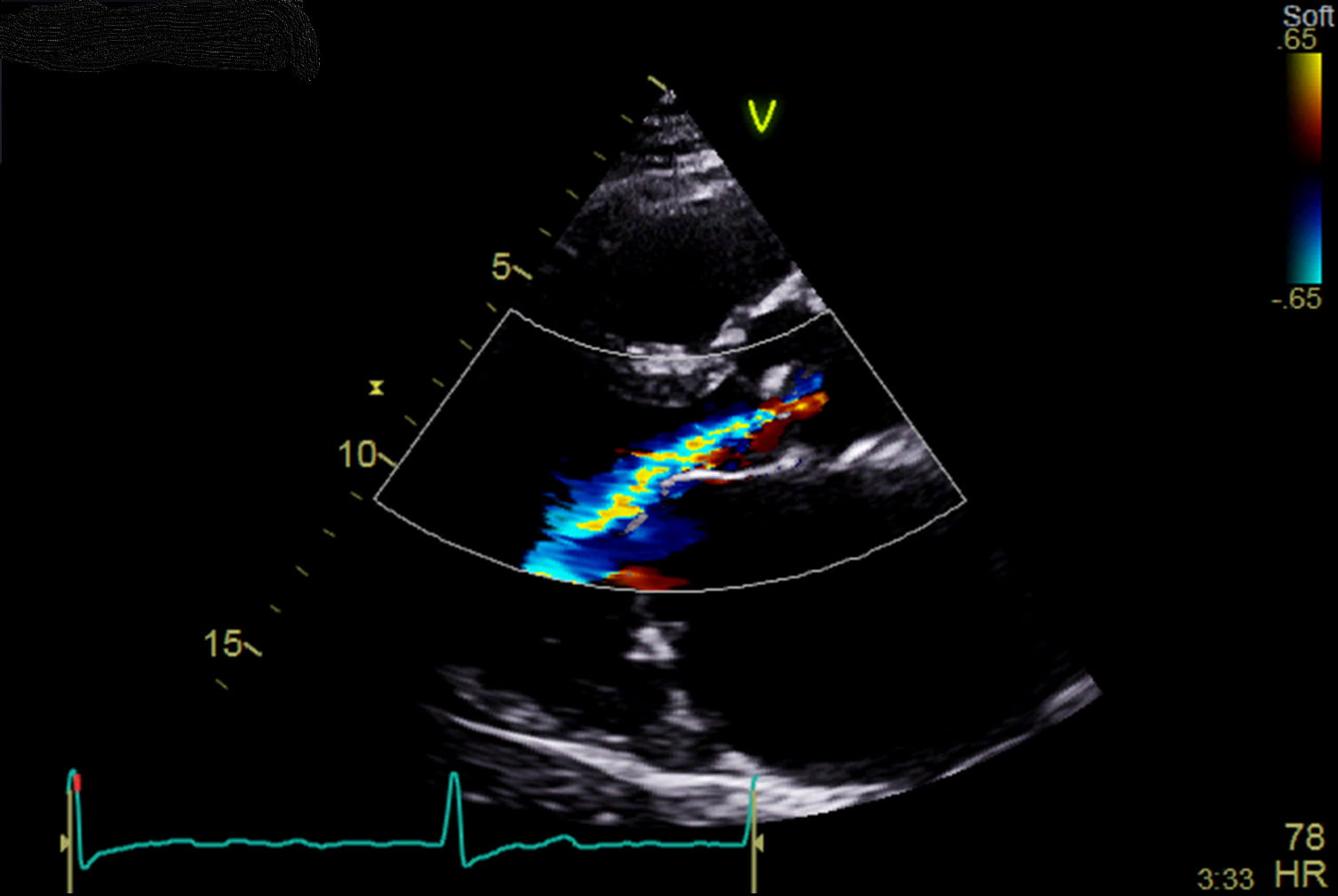
Valve regurgitation is a condition where one or more of the heart valves do not close properly, allowing blood to flow backwards instead of moving forward through the heart and into the rest of the body.
This can place extra stress on the heart and may lead to serious cardiovascular complications if left untreated. This page explores the key aspects of valve regurgitation, including its definition, types, severity, symptoms, causes, and available treatments. Additionally, we will discuss the vital role of heart scans in diagnosing valve regurgitation and emphasise the importance of seeking care from a professional cardiac clinic.
What is Valve Regurgitation?
Valve regurgitation, also known as valvular insufficiency or incompetence, occurs when a heart valve fails to close completely, allowing blood to leak back through the valve. The heart consists of four valves - the aortic, mitral, pulmonary, and tricuspid valves - which are responsible for maintaining the correct direction of blood flow.
When one of these valves becomes regurgitant, it disrupts the normal flow of blood, leading to a decrease in the efficiency of the heart's pumping action. This condition can vary in severity, and over time, it may contribute to heart enlargement, heart failure, or other serious complications.
How Serious Is It? & Are There Different Types?
The seriousness of valve regurgitation can vary significantly based on the valve affected and the degree of leakage. Valve regurgitation is classified into different types depending on the specific valve involved:
- Mitral Regurgitation: This occurs when the mitral valve, located between the left atrium and left ventricle, does not close properly, causing blood to flow backwards into the left atrium. It is the most common type of valve regurgitation and can lead to symptoms such as shortness of breath and fatigue.
- Aortic Regurgitation: This happens when the aortic valve, which controls blood flow from the left ventricle into the aorta, fails to close tightly, allowing blood to leak back into the left ventricle. Aortic regurgitation can result in symptoms like chest pain and shortness of breath, particularly during physical activity.
- Tricuspid Regurgitation: In this type, the tricuspid valve, located between the right atrium and right ventricle, does not close properly, causing blood to flow back into the right atrium. Tricuspid regurgitation often accompanies other valve issues or heart conditions.
- Pulmonary Regurgitation: This occurs when the pulmonary valve, which regulates blood flow from the right ventricle to the pulmonary artery, does not close completely. Pulmonary regurgitation is less common and usually results from conditions such as pulmonary hypertension or congenital heart defects.
Symptoms
The symptoms of valve regurgitation depend on the severity of the condition and the valve affected. Some people with mild regurgitation may not experience symptoms, while others with more severe cases may exhibit the following:
- Shortness of breath: Often worse during physical activity or when lying down.
- Fatigue: A feeling of extreme tiredness, especially during exertion.
- Heart palpitations: Sensations of a racing, fluttering, or irregular heartbeat.
- Swelling: Particularly in the legs, ankles, and feet, due to fluid buildup.
- Chest pain: A tight, squeezing pain, especially with aortic regurgitation.
- Lightheadedness or fainting: Caused by inadequate blood flow to the brain.
Causes
Valve regurgitation can result from a variety of underlying conditions or factors:
- Congenital heart defects: Some people are born with valve abnormalities that lead to regurgitation.
- Rheumatic fever: An inflammatory disease that can develop after untreated strep throat, leading to valve damage.
- Endocarditis: An infection of the inner lining of the heart, which can damage the heart valves.
- Heart valve prolapse: A condition where the valve flaps bulge back into the heart chamber, leading to incomplete closure.
- Heart attack: Can damage the heart muscle and affect the function of the valves.
- Hypertension: Chronic high blood pressure can lead to valve damage over time.
- Ageing: Degenerative changes in the valve structure as a person ages can lead to regurgitation.
Available Treatments
Treatment for valve regurgitation depends on the severity of the condition and its underlying cause. Options include:
- Medications: Although medications cannot cure valve regurgitation, they can help manage symptoms and prevent complications. These may include diuretics to reduce fluid buildup, vasodilators to lower blood pressure, and beta-blockers to regulate heart rate.
- Valve Repair: In some cases, valves can be surgically repaired to improve their function. This may involve reshaping the valve, removing excess tissue, or repairing valve flaps.
- Valve Replacement: In more severe cases, the damaged valve may need to be replaced with a mechanical or biological valve through surgery.
- Transcatheter Procedures: For patients who are not candidates for traditional surgery, minimally invasive procedures like Transcatheter Aortic Valve Replacement (TAVR) may be an option.
The Role of Heart Scans in Identifying The Issue
Heart scans are crucial for diagnosing valve regurgitation and assessing its severity. These imaging tests allow cardiologists to visualise the heart valves, measure the degree of regurgitation, and evaluate the heart's overall function. Common heart scans used include:
- Echocardiogram: An ultrasound of the heart that provides detailed images of the heart valves in motion, helping to identify the extent of regurgitation.
- Cardiac MRI: Offers a more comprehensive view of the heart’s structure and function, including precise measurements of blood flow and valve function.
- CT Scans: These can be used to visualise the heart valves and detect structural abnormalities that may contribute to regurgitation.
- Cardiac Catheterisation: This procedure involves inserting a catheter into the heart’s blood vessels to measure pressures within the heart chambers and evaluate the severity of valve regurgitation.
The Importance of Trusting a Professional Cardiac Clinic
Given the complexity and potential severity of valve regurgitation, it is essential to seek care from a professional cardiac clinic with experienced cardiologists and access to advanced diagnostic tools. A specialised cardiac clinic can provide accurate diagnoses, develop personalised treatment plans, and offer ongoing care to manage the condition effectively.
Trusting a professional cardiac clinic ensures that patients receive the highest standard of care, which is critical for preventing complications, improving symptoms, and enhancing long-term outcomes.
In summary, valve regurgitation is a serious heart condition that requires careful monitoring and appropriate treatment. Understanding its symptoms, causes, and treatment options, along with the importance of professional care, is essential for managing the condition effectively and maintaining a better quality of life.
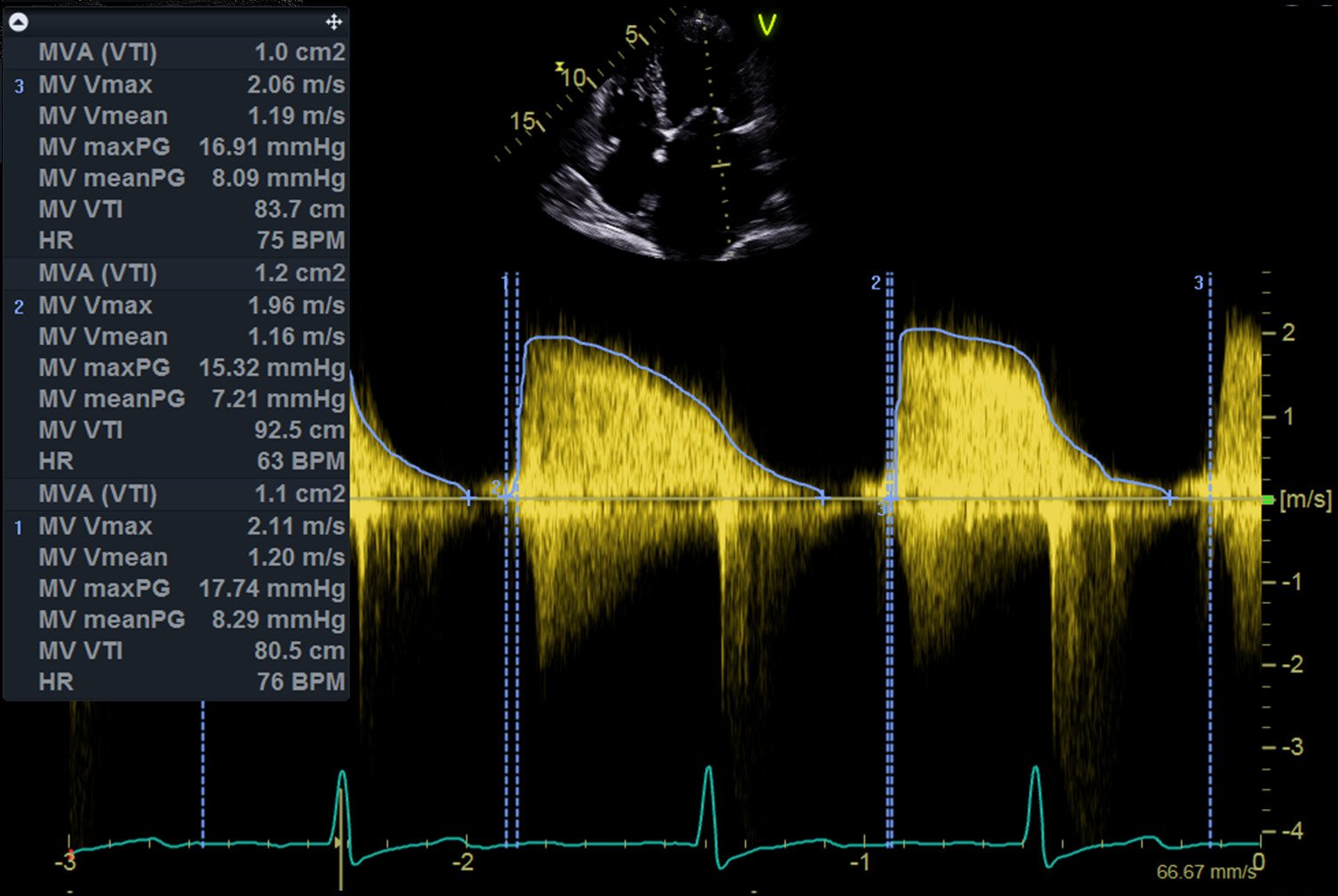
Valve Stenosis is a heart condition that affects the normal functioning of the heart valves and can significantly impact the heart's ability to pump blood efficiently, leading to various health complications. This page covers the essential aspects of Valve Stenosis, including its definition, types, seriousness, symptoms, causes, and treatments.
We also discuss the role of heart scans in diagnosing this condition and the importance of seeking care from a professional cardiac clinic.
What is Valve Stenosis?
Valve Stenosis refers to the narrowing of one of the heart's valves, which restricts blood flow. The heart has four valves—the aortic, mitral, pulmonary, and tricuspid - that ensure blood flows in the right direction through the heart's chambers and into the rest of the body.
When one of these valves becomes stenotic (narrowed), it creates an obstruction, which forces the heart to work harder to pump blood. Over time, this increased workload can weaken the heart, leading to more severe cardiovascular issues.
How Serious Is It? & Are There Different Types?
Valve Stenosis can range from mild to severe, depending on the degree of narrowing and the valve affected. The seriousness of the condition is generally classified as mild, moderate, or severe.
- Mild Valve Stenosis: In mild cases, the narrowing of the valve is slight, and it may not cause significant symptoms. However, it requires regular monitoring to ensure it doesn't progress.
- Moderate Valve Stenosis: This level of stenosis may cause noticeable symptoms and affect the heart’s function. Treatment may be necessary to manage the condition and prevent it from worsening.
- Severe Valve Stenosis: Severe stenosis can lead to significant heart problems, including heart failure. This level of stenosis often requires surgical intervention to repair or replace the affected valve.
The most common types of Valve Stenosis are:
- Aortic Stenosis: The narrowing of the aortic valve, which restricts blood flow from the left ventricle to the aorta and the rest of the body.
- Mitral Stenosis: The narrowing of the mitral valve, which restricts blood flow from the left atrium to the left ventricle.
- Pulmonary Stenosis: The narrowing of the pulmonary valve, which restricts blood flow from the right ventricle to the pulmonary artery and the lungs.
- Tricuspid Stenosis: The narrowing of the tricuspid valve, which restricts blood flow from the right atrium to the right ventricle.
Symptoms
The symptoms of Valve Stenosis vary depending on the severity of the condition and the valve affected. Common symptoms include:
- Shortness of breath: Especially during physical activity.
- Chest pain: Often described as angina, a squeezing or pressure-like pain in the chest.
- Fatigue: A general feeling of tiredness, especially after exertion.
- Palpitations: A sensation of irregular or fast heartbeats.
- Dizziness or fainting: Particularly during exertion, which may indicate severe aortic stenosis.
- Swelling: Particularly in the legs and feet, due to fluid buildup.
Causes
Several factors can lead to Valve Stenosis, including:
- Congenital defects: Some people are born with heart valve abnormalities that may lead to stenosis over time.
- Age-related changes: As people age, calcium deposits can build up on the heart valves, leading to stiffening and narrowing.
- Rheumatic fever: A complication of untreated strep throat, which can cause inflammation and scarring of the heart valves, leading to stenosis.
- Radiation therapy: Treatment for cancers in the chest area can sometimes damage the heart valves, leading to stenosis.
Available Treatments
Treatment for Valve Stenosis depends on the severity of the condition and the patient’s overall health. Options include:
- Medications: While medications cannot cure Valve Stenosis, they can manage symptoms and prevent complications. These might include diuretics to reduce fluid buildup, beta-blockers to lower heart rate, and anticoagulants to prevent blood clots.
- Balloon Valvuloplasty: A minimally invasive procedure where a balloon is inserted into the narrowed valve and inflated to widen the opening.
- Valve Repair or Replacement Surgery: In severe cases, surgery may be required to repair or replace the stenotic valve with a mechanical or biological valve.
The Role of Heart Scans in Identifying The Issues
Heart scans play a critical role in diagnosing Valve Stenosis, allowing cardiologists to assess the structure and function of the heart valves and determine the severity of the stenosis. The common types of heart scans used in the diagnosis include:
- Echocardiogram: An ultrasound of the heart that provides detailed images of the heart valves, allowing the doctor to see how well the valves are opening and closing.
- Cardiac MRI: A detailed scan that provides comprehensive images of the heart’s structure and function.
- CT Scan: A high-resolution scan that can show calcium deposits on the valves and help assess the severity of the stenosis.
- Cardiac Catheterisation: A procedure where a catheter is inserted into the heart’s blood vessels to measure the pressure inside the heart chambers and across the stenotic valve.
The Importance of Trusting A Professional Cardiac Clinic
Given the complexities and potential severity of Valve Stenosis, it's crucial to seek care from a professional cardiac clinic with experienced cardiologists and access to advanced diagnostic tools. A professional cardiac clinic can provide an accurate diagnosis, personalised treatment plans, and ongoing care to manage the condition effectively. Trusting a specialised clinic ensures that patients receive the highest standard of care, which is essential for preventing complications and improving long-term outcomes.
In summary, Valve Stenosis is a very serious heart condition that requires careful management and treatment. Understanding the symptoms, causes, and treatment options, along with the importance of professional care, can help individuals manage the condition effectively and maintain a better quality of life.
The left ventricle pumps blood through the aortic valve and into the aorta, which is the body’s largest artery. An echo scan can assess the size of and blood flow through the early part of the aorta. A number of conditions – such as high blood pressure or aortic valve problems – can cause the aorta to enlarge (or ‘dilate’) over time. A mildly dilated aorta is often seen in older people, or people with high blood pressure, and may not cause significant problems, however a severely dilated aorta will need specialist follow-up, and may ultimately need an operation to repair or replace this important blood vessel.
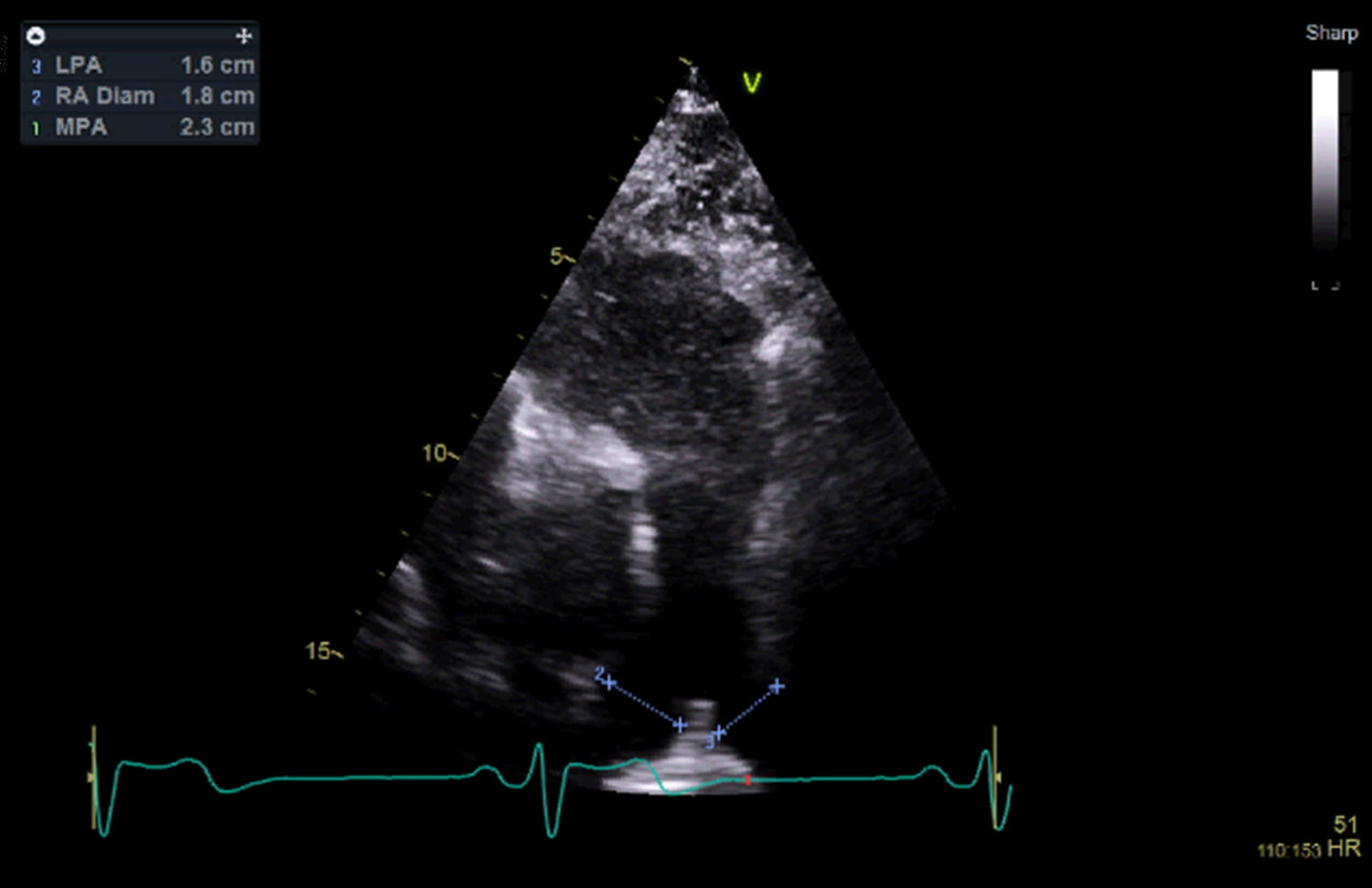
The pulmonary arteries are critical components of the cardiovascular system, responsible for transporting deoxygenated blood from the right ventricle of the heart to the lungs for oxygenation.
This page provides an in-depth overview of the pulmonary arteries, their definition, the seriousness and types of conditions affecting them, symptoms, causes, treatments, the role of heart scans in diagnosis, and the importance of seeking care from a professional cardiac clinic.
Blood Vessels: The Pulmonary Arteries
The pulmonary arteries originate from the right ventricle of the heart, consisting of the main pulmonary artery, which bifurcates into the left and right pulmonary arteries.
The main pulmonary artery arises from the pulmonary valve, splitting into the left and right pulmonary arteries at the pulmonary trunk, responsible for transporting deoxygenated blood to the respective lungs.
How serious are Pulmonary Artery Conditions?
Conditions affecting the pulmonary arteries can be severe and life-threatening. The most significant conditions include:
- Pulmonary Arterial Hypertension (PAH): A type of high blood pressure that affects the arteries in the lungs and the right side of the heart. PAH can lead to right heart failure if left untreated.
- Pulmonary Embolism: A blockage in one of the pulmonary arteries, usually due to blood clots that travel to the lungs from the legs (deep vein thrombosis).
- Enlarged Pulmonary Artery: Also known as pulmonary artery dilation, this can be due to various causes, including PAH, congenital heart disease, or chronic lung disease.
Symptoms
The symptoms of pulmonary artery conditions can vary, but common symptoms include:
- Shortness of Breath: Especially during physical activity.
- Fatigue: Due to reduced oxygen delivery to tissues.
- Chest Pain: Particularly in PAH, where the heart has to work harder.
- Palpitations: Irregular heartbeats due to increased cardiac workload.
- Dizziness or Fainting: Due to inadequate blood flow and oxygen delivery.
- Swelling in the Ankles or Abdomen: Indicating right heart failure.
Causes
The causes of pulmonary artery conditions are diverse and include:
- Pulmonary Arterial Hypertension (PAH): Causes can be idiopathic (unknown), genetic, or secondary to other conditions such as connective tissue diseases, congenital heart diseases, chronic liver disease, or HIV infection.
- Pulmonary Embolism: Typically caused by blood clots originating from the legs or other parts of the body that travel to the lungs.
- Enlarged Pulmonary Artery: This can result from long-standing PAH, congenital heart defects, or chronic lung diseases like chronic obstructive pulmonary disease (COPD).
Treatments
Treatment for pulmonary artery conditions varies based on the specific issue:
- Pulmonary Arterial Hypertension (PAH):
- Medications: Include endothelin receptor antagonists, phosphodiesterase-5 inhibitors, and prostacyclin analogues to relax and widen the pulmonary arteries.
- Lifestyle Changes: Such as low-sodium diets and regular, moderate exercise.
- Oxygen Therapy: To improve oxygen levels in the blood.
- Surgical Options: In severe cases, lung or heart-lung transplantation may be considered.
- Pulmonary Embolism:
- Anticoagulation Therapy: Blood thinners like heparin and warfarin to prevent new clots from forming.
- Thrombolytic Therapy: Clot-dissolving medications for severe cases.
- Surgical or Catheter-Based Procedures: To remove the clot in emergency situations.
- Enlarged Pulmonary Artery:
- Managing Underlying Conditions: Such as treating PAH or chronic lung diseases.
- Regular Monitoring: Through imaging tests to track changes in the artery size.
The role of heart scans in identifying pulmonary artery issues
Heart scans are essential for diagnosing pulmonary artery conditions:
- Echocardiogram: Uses sound waves to create images of the heart and can assess the size and function of the pulmonary arteries and right ventricle.
- CT Pulmonary Angiography: Provides detailed images of the pulmonary arteries to detect blockages or other abnormalities.
- MRI: Offers high-resolution images and is particularly useful for detailed assessment of the heart and pulmonary vessels.
- Right Heart Catheterization: A procedure that measures pressures within the pulmonary arteries and right side of the heart, essential for diagnosing PAH.
The importance of trusting an expert Cardiac Clinic
Seeking care from a professional cardiac clinic is crucial for managing pulmonary artery conditions effectively. The benefits include:
- Expertise: Cardiologists and pulmonologists with specialised knowledge and experience in diagnosing and treating complex pulmonary artery conditions.
- Advanced Diagnostic Tools: Access to state-of-the-art imaging technologies and diagnostic equipment ensures accurate assessments.
- Comprehensive Care: Multidisciplinary teams provide holistic care, addressing all aspects of a patient's health and condition.
- Personalised Treatment Plans: Tailored to individual needs, ensuring the best possible outcomes.
- Ongoing Monitoring and Follow-up: Regular check-ups and monitoring to detect any recurrence or complications early, providing timely interventions.
- Patient Education and Support: Ensuring patients understand their condition, treatment options, and lifestyle changes needed to manage their health effectively.
For more information on our services, contact our helpful and friendly team today, or alternatively, you can book an appointment at one of our specialist clinics online now.
Conclusion
The pulmonary arteries play a vital role in the cardiovascular system, transporting deoxygenated blood from the heart to the lungs for oxygenation. Conditions such as pulmonary arterial hypertension, pulmonary embolism, and enlarged pulmonary artery can be serious and require prompt diagnosis and treatment. Symptoms can include shortness of breath, fatigue, chest pain, and swelling in the lower extremities.
Heart scans and other imaging techniques are crucial for accurately diagnosing these conditions and guiding treatment decisions. Trusting a professional cardiac clinic ensures that patients receive expert care, benefiting from specialised knowledge, advanced technology, comprehensive care, and personalised treatment plans. By seeking care from specialist professionals, patients can achieve better health outcomes and effectively manage the risks associated with pulmonary artery conditions.
The cardiovascular system is a complex network of blood vessels that are responsible for transporting blood throughout the body, with the inferior vena cava (IVC) playing a critical role among these vessels.
This page provides a comprehensive overview of the IVC, including its definition, function, potential health issues, symptoms, causes, treatments, and the importance of accurate diagnosis and treatment by a professional cardiac clinic.
Blood Vessels: What is the Inferior Vena Cava?
The inferior vena cava is one of the largest veins in the human body and is a vital component of the circulatory system, responsible for returning deoxygenated blood from the lower half of the body to the heart.
The IVC is formed by the confluence of the left and right common iliac veins, which drain blood from the lower limbs and pelvis. It ascends along the right side of the vertebral column, passes through the diaphragm, and empties into the right atrium of the heart, hence, it can be visualised and assessed during an echocardiogram.
Which conditions affect the Inferior Vena Cava?
Conditions affecting the inferior vena cava can be serious and potentially life-threatening, with the most common issues including:
- Inferior Vena Cava Obstruction: A blockage in the IVC can lead to severe complications. This obstruction can be caused by thrombosis (blood clots), tumours, or external compression from adjacent structures.
- Inferior Vena Cava Thrombosis: A specific type of IVC obstruction caused by blood clots. This condition is serious because it can lead to reduced blood flow back to the heart, causing swelling and pain in the lower extremities.
- Inferior Vena Cava Collapse: A condition where the IVC partially or completely collapses due to external compression, dehydration, or severe blood loss, significantly affecting blood circulation.
Symptoms
Symptoms of IVC-related conditions can vary depending on the specific issue but often include:
- Swelling and Oedema: Particularly in the lower extremities, due to impaired blood return.
- Pain: In the legs or lower back, which may indicate thrombosis or obstruction.
- Shortness of Breath: If a thrombus dislodges and travels to the lungs, causing a pulmonary embolism.
- Abdominal Pain: Particularly if the obstruction is caused by a tumour or external compression.
- Fatigue and Weakness: Due to compromised circulation and reduced oxygen delivery to tissues.
- Symptoms of Inferior Vena Cava Collapse: Dizziness, hypotension, and signs of shock in severe cases.
Causes
The causes of inferior vena cava obstruction and related conditions include:
- Thrombosis: Blood clots can form within the IVC, obstructing blood flow, which can be due to hypercoagulable states, prolonged immobility, or certain medical conditions.
- Tumours: Both primary tumours and metastases can compress or invade the IVC, leading to obstruction.
- Congenital Abnormalities: Some individuals are born with structural abnormalities that predispose them to IVC-related issues.
- External Compression: From adjacent structures, such as enlarged livers, lymph nodes, or abdominal masses.
- Trauma: Injuries to the abdomen or pelvis can damage the IVC.
Treatments
Treatment for IVC-related conditions varies based on the specific issue:
- Anticoagulation Therapy: Used for IVC thrombosis, anticoagulants like heparin or warfarin are commonly used to prevent further clot formation and promote clot dissolution.
- Thrombolytic Therapy: In severe cases of thrombosis, clot-dissolving medications may be administered.
- Surgical Interventions: For obstructions caused by tumours or congenital abnormalities, surgery may be necessary to remove the obstruction or repair the IVC.
- IVC Filters: In some cases, a filter is placed in the IVC to prevent blood clots from travelling to the lungs.
- Management of Underlying Conditions: Treating the primary cause, such as cancer or an infection, can alleviate the IVC obstruction.
- Lifestyle Changes and Supportive Care: Including hydration, compression stockings, and physical activity to improve circulation and reduce symptoms.
The role of heart scans in identifying the issues
Heart scans and other imaging techniques are crucial in diagnosing conditions related to the inferior vena cava. These methods include:
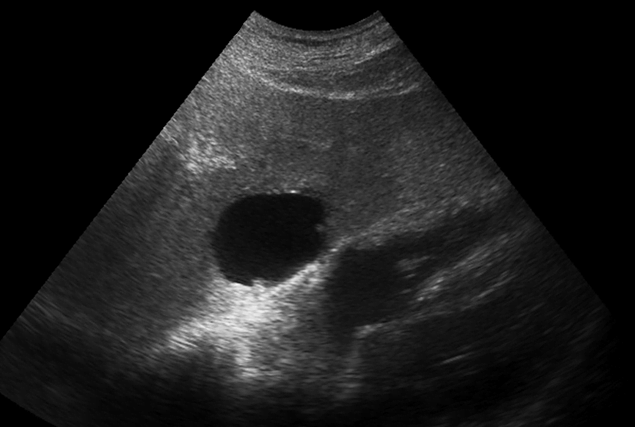
- Ultrasound: A non-invasive test that uses sound waves to create images of the blood vessels, helping to detect thrombi and assess blood flow.
- CT Scan: Provides detailed cross-sectional images of the body, allowing visualisation of the IVC and identification of obstructions, tumours, or structural abnormalities.
- MRI: Offers high-resolution images of the blood vessels and surrounding tissues, useful for detailed assessment of the IVC.
- Venography: An invasive procedure where contrast dye is injected into the veins, and X-ray images are taken to visualise the IVC and detect blockages or abnormalities.
The importance of trusting an expert Cardiac Clinic
Accurate diagnosis and effective treatment of IVC-related conditions require the expertise of a professional cardiac clinic. The benefits of consulting a specialised clinic include:
- Expertise: Cardiologists and vascular specialists with extensive experience diagnosing and managing complex vascular conditions.
- Advanced Diagnostic Tools: Access to state-of-the-art imaging technologies and diagnostic equipment ensures accurate assessments.
- Comprehensive Care: Multidisciplinary teams provide holistic care, addressing all aspects of the patient's health and condition.
- Personalised Treatment Plans: Tailored to each patient's specific needs and medical history, ensuring the best possible outcomes.
- Ongoing Monitoring and Follow-up: Regular check-ups and monitoring to detect any recurrence or complications early, providing timely interventions.
- Patient Education and Support: Ensuring patients understand their condition, treatment options, and lifestyle changes needed to manage their health effectively.
For more information on our services, contact our helpful and friendly team today, or alternatively, you can book an appointment at one of our specialist clinics online now.
Conclusion
The inferior vena cava is a vital component of the circulatory system, responsible for returning deoxygenated blood from the lower half of the body to the heart. Conditions affecting the IVC, such as obstruction, thrombosis, and collapse, can be serious and require timely diagnosis and treatment. Symptoms can range from swelling and pain to shortness of breath and fatigue, while causes include thrombosis, tumours, congenital abnormalities, external compression, and trauma.
Heart scans and other imaging techniques play a crucial role in identifying IVC-related issues, providing detailed visualisations that guide treatment decisions. Trusting a professional cardiac clinic ensures that patients receive expert care, benefiting from specialised knowledge, advanced technology, comprehensive care, and personalised treatment plans. By seeking care from specialised professionals, patients can achieve better health outcomes and effectively manage the risks associated with inferior vena cava conditions.
The pericardium is a double-layered sac that surrounds and protects the heart, playing a crucial role in maintaining the heart's position within the chest and reducing friction between the heart and surrounding structures as it beats.
This page covers the anatomy and function of the pericardium, various conditions affecting it, their seriousness, symptoms, causes, treatments, the role of heart scans in identifying these issues, and the importance of consulting a professional cardiac clinic for accurate diagnosis and effective treatment.
What is the Pericardium?
The pericardium consists of two distinct layers:
- Fibrous Pericardium: The tough outer layer anchoring the heart to the diaphragm, sternum, and surrounding tissues.
- Serous Pericardium: The inner layer that is further divided into:
- Parietal Layer: Lines the inner surface of the fibrous pericardium.
- Visceral Layer (Epicardium): Adheres closely to the heart muscle.
Between these layers is the pericardial cavity, which contains a small amount of lubricating fluid that minimises friction during heartbeats.
How serious are Pericardial Conditions? & Are there different types?
Pericardial conditions can range from mild to life-threatening, depending on the type and severity.
Key conditions include:
- Pericarditis: Inflammation of the pericardium, which can be acute or chronic.
- Pericardial Effusion: Accumulation of excess fluid in the pericardial cavity.
- Constrictive Pericarditis: Chronic inflammation leading to thickening and scarring of the pericardium, restricting heart movement.
- Cardiac Tamponade: A severe complication of pericardial effusion where excess fluid compresses the heart, impairing its ability to pump blood effectively.
Symptoms
Symptoms of pericardial conditions vary but often include:
- Chest Pain: Sharp or stabbing pain that may worsen with deep breathing or lying down, commonly associated with pericarditis.
- Shortness of Breath: Particularly with pericardial effusion or cardiac tamponade due to impaired heart function.
- Heart Palpitations: Irregular heartbeats can occur in response to inflammation or fluid buildup.
- Fatigue and Weakness: General malaise due to reduced cardiac efficiency.
- Swelling: In the legs or abdomen, indicating fluid retention and heart failure in severe cases.
- Low-Grade Fever: Common in inflammatory conditions like pericarditis.
Causes
The causes of pericardial conditions are varied and include:
- Infections: Viral infections (e.g., Coxsackievirus), bacterial infections (e.g., tuberculosis), and fungal infections can lead to pericarditis.
- Autoimmune Disorders: Conditions like lupus and rheumatoid arthritis can cause pericardial inflammation.
- Heart Attack: Damage to the heart muscle can trigger pericardial inflammation.
- Trauma: Injury to the chest can lead to pericardial effusion or inflammation.
- Cancer: Both primary tumours of the pericardium and metastatic cancer can cause pericardial effusion.
- Medical Procedures: Complications from heart surgery or radiation therapy.
Treatments
Treatment for pericardial conditions depends on the specific diagnosis and severity:
- Medications:
- Anti-inflammatory Drugs: NSAIDs (such as Ibuprofen) and colchicine for managing pericarditis.
- Antibiotics or Antifungals: For infections causing pericarditis or pericardial effusion.
- Corticosteroids: For severe or recurrent pericarditis, especially when autoimmune diseases are involved.
- Procedures:
- Pericardiocentesis: Draining excess fluid in cases of pericardial effusion or cardiac tamponade.
- Pericardiectomy: Surgical removal of the pericardium in severe cases of constrictive pericarditis.
- Monitoring and Supportive Care:
- Rest and Activity Modification: Essential during acute episodes of pericarditis.
- Close Monitoring: For signs of complications like cardiac tamponade.
The role of heart scans in identifying Pericardial Disease
Heart scans are critical in diagnosing pericardial conditions accurately:
- Echocardiogram: The primary tool for assessing pericardial effusion and cardiac tamponade. It visualises fluid accumulation and heart function.
- Electrocardiogram (ECG): Used to detect pericarditis. Pericarditis ECG findings include diffuse ST-segment elevation and PR-segment depression.
- Chest X-ray: Can show an enlarged heart silhouette if significant pericardial effusion is present.
- Cardiac MRI and CT: Provide detailed images of the pericardium, helping to diagnose conditions like constrictive pericarditis and pericardial tumours.
The importance of trusting a professional Cardiac Clinic
Consulting a professional cardiac clinic is crucial for managing pericardial conditions effectively.
The benefits include:
- Expertise: Cardiologists and cardiac surgeons have specialised knowledge and experience in diagnosing and treating pericardial diseases.
- Advanced Technology: Access to state-of-the-art diagnostic tools and treatment options ensures accurate assessment and effective intervention.
- Comprehensive Care: Multidisciplinary teams provide holistic care, addressing all aspects of a patient's condition.
- Personalised Treatment Plans: Tailored to individual needs, ensuring the best possible outcomes.
- Ongoing Monitoring: Regular follow-ups and monitoring to detect and manage any recurrence or complications early.
For more information on our services, contact our helpful and friendly team today, or alternatively, you can book an appointment at one of our specialist clinics online now.
Conclusion
The pericardium is a vital structure that protects and supports the heart. The conditions affecting the pericardium, such as pericarditis, pericardial effusion, and constrictive pericarditis, can range from mild to life-threatening.
Understanding the symptoms, causes, and treatments of these conditions is crucial for effective management. Heart scans play a pivotal role in diagnosing pericardial issues, providing detailed images that guide treatment decisions.
Trusting a professional cardiac clinic ensures that patients receive the highest standard of care, benefiting from specialised expertise, advanced technology, comprehensive care, and personalised treatment plans. By seeking care from specialised professionals, patients can achieve better health outcomes and effectively manage the risks associated with pericardial conditions.
Masses attached to heart valves are abnormal growths or formations that can develop on the heart valves, significantly impacting cardiovascular function.
This page provides a comprehensive overview of such masses, including their nature, seriousness, symptoms, causes, treatments, the role of heart scans in diagnosis, and the importance of consulting a professional cardiac clinic.
What are masses attached to valves?
Masses attached to heart valves are abnormal tissue growths or thrombi that adhere to the valve structures. These masses can be benign or malignant and include a variety of forms, such as:
- Valvular Tumours: Both benign (e.g., papillary fibroelastomas, myxomas) and malignant (e.g., sarcomas).
- Vegetations: Infectious masses, typically seen in conditions like infective endocarditis.
- Thrombi: Blood clots forming on valves, often due to turbulent blood flow or underlying heart conditions.
How serious are they? & Are there different types?
The seriousness of masses attached to valves depends on their type, size, and location:
- Benign Tumours:
- Papillary Fibroelastomas: These are the most common benign valvular tumours, usually attached to the aortic or mitral valves. They can cause embolic events but are generally considered less aggressive.
- Valvular Myxomas: Though more common in atrial chambers, they can occasionally attach to valves and cause significant obstruction or embolism.
- Malignant Tumours:
- Sarcomas: Rare but highly aggressive, they can invade nearby structures and metastasize, leading to poor prognosis.
- Vegetations:
- Seen in infective endocarditis, these masses can cause severe valve damage, leading to valve dysfunction, systemic embolism, and sepsis.
- Thrombi:
- These can obstruct blood flow or embolize, causing strokes or other ischemic events. They are often associated with atrial fibrillation or mechanical heart valves.
Symptoms
The symptoms of masses attached to heart valves can vary widely based on the type and size of the mass:
- Chest Pain: Especially if the mass obstructs blood flow.
- Shortness of Breath: Due to impaired valve function leading to heart failure.
- Palpitations: Irregular heart rhythms caused by disrupted blood flow.
- Fever and Malaise: Common in infective endocarditis due to infection.
- Stroke or Transient Ischemic Attack (TIA): Resulting from emboli breaking off and travelling to the brain.
- Fatigue and Weakness: From reduced cardiac output and systemic embolism.
Causes
The causes of masses attached to valves vary:
- Infective Endocarditis: Bacterial or fungal infections can lead to the formation of vegetation on heart valves.
- Genetic Factors: Some benign tumours like myxomas may have a genetic predisposition.
- Underlying Heart Conditions: Conditions such as atrial fibrillation can lead to thrombus formation on valves.
- Cancer: Primary or metastatic malignancies can involve heart valves.
Treatments
Treatment for masses attached to valves depends on the type and severity of the mass:
- Surgical Removal:
- Tumour Resection: Surgical removal of benign or malignant tumours.
- Valve Replacement or Repair: In cases where the valve is significantly damaged.
- Antibiotic Therapy:
- Essential for treating infective endocarditis to eradicate the infection and reduce vegetation size.
- Anticoagulation Therapy:
- Used to treat and prevent thrombi, especially in patients with atrial fibrillation or mechanical valves.
- Chemotherapy and Radiation:
- For malignant tumours, adjunctive therapies may be necessary.
The role of heart scans in identifying the issue
Heart scans are vital in diagnosing and managing masses attached to heart valves, with advanced imaging techniques providing detailed visualisation of the heart's structure, facilitating accurate diagnosis and treatment planning:
- Echocardiogram:
- Transthoracic Echocardiography (TTE): A non-invasive test that uses sound waves to create images of the heart, often the first-line imaging technique.
- Transesophageal Echocardiography (TEE): Provides more detailed images by inserting an ultrasound probe into the oesophagus closer to the heart valves.
- Cardiac MRI:
- Offers high-resolution images of the heart's structure and function, useful for distinguishing between different types of masses.
- CT Scan:
- Provides detailed cross-sectional images and can be used to assess the extent of tumour invasion or the presence of calcifications.
- PET Scan:
- Helps in identifying malignant tumours and assessing their metabolic activity.
The importance of trusting a professional Cardiac Clinic
Given the complexity and potential severity of masses attached to heart valves, seeking care from a specialised cardiac clinic is vital. Professional cardiac clinics offer several advantages:
- Expertise:
- Cardiologists, cardiothoracic surgeons, and other specialists have the expertise to accurately diagnose and treat these conditions effectively.
- Advanced Technology:
- Access to state-of-the-art diagnostic tools and treatment technologies ensures precise assessments and interventions.
- Comprehensive Care:
- Multidisciplinary teams provide holistic care, addressing all aspects of a patient’s health, from initial diagnosis to post-treatment follow-up.
- Personalised Treatment Plans:
- Individualised care plans tailored to each patient's specific needs and conditions ensure optimal outcomes.
- Ongoing Monitoring:
- Regular follow-ups and imaging tests to monitor for recurrence or complications are essential for the long-term management of valve masses.
For more information on our services, contact our helpful and friendly team today, or alternatively, you can book an appointment at one of our specialist clinics online now.
Conclusion
Masses attached to heart valves, whether benign tumours, malignant tumours, vegetations from infective endocarditis or thrombi, are significant health concerns, requiring timely and accurate diagnosis. Symptoms can range from chest pain and shortness of breath to systemic embolic events like strokes.
Causes vary from infections and genetic factors to underlying heart conditions and cancer. Treatments include surgical removal, antibiotic therapy, anticoagulation, and adjunctive therapies for malignancies.
Heart scans play a crucial role in diagnosing these masses, providing detailed images that guide effective treatment planning. Trusting a professional cardiac clinic ensures that patients receive the highest standard of care, benefiting from specialised expertise, advanced technology, comprehensive care, and personalised treatment plans.
Seeking care from a specialised professional means patients can achieve better health outcomes and effectively manage the risks associated with these potentially life-threatening conditions.
Primary cardiac tumours – such as a left atrial ‘myxoma’ – are extremely rare. If your scan is suspicious for a tumour, you will be referred for specialist investigation.
A blood clot – or ‘thrombus’ – is an unusual finding in the heart, but can be encountered in patients with a recent heart attack, or in cases of very severely reduced systolic function. These cases will need referral for consideration of blood thinning medication. Very small blood clots can be difficult to see on a standard cardiac ultrasound; if there is any doubt, you may be referred for consideration of an alternative imaging test.
Abnormalities outside of the heart, also known as extracardiac abnormalities, refers to the various conditions affecting the blood vessels, structures, and tissues surrounding the heart.
These abnormalities can significantly impact cardiovascular health, contributing to or exacerbating heart disease.
This page explores the nature of these abnormalities, their seriousness, symptoms, causes, treatments, and the role of heart scans in diagnosing these conditions. Additionally, we highlight the importance of consulting a professional cardiac clinic for proper diagnosis and treatment.
What are abnormalities outside of the heart?
Extracardiac abnormalities encompass a range of conditions affecting the major blood vessels (such as the aorta and pulmonary arteries), the pericardium (the protective sac around the heart), and other structures like the thoracic cavity and diaphragm.
Common examples include aortic aneurysms, pulmonary embolisms, and pericardial effusion. These conditions can compromise the heart's ability to function correctly, leading to severe health consequences if not appropriately managed.
How serious is it? & Are there different types?
The seriousness of abnormalities outside the heart varies significantly depending on the specific condition and its severity. Here are a few types:
- Aortic Aneurysms: This condition involves the abnormal bulging of the aorta, the main artery carrying blood from the heart to the rest of the body. If an aneurysm ruptures, it can lead to life-threatening internal bleeding.
- Pulmonary Embolism: A blockage in one of the pulmonary arteries in the lungs, usually caused by blood clots that travel from the legs (deep vein thrombosis). This condition can be fatal if not treated promptly.
- Pericardial Effusion: The accumulation of excess fluid in the pericardium, which can compress the heart and impair its function, leading to a condition called cardiac tamponade.
- Coarctation of the Aorta: A congenital condition characterised by the narrowing of the aorta, which can increase blood pressure and strain on the heart.
- Liver Lesions: The liver is partially visualised during a cardiac ultrasound; this may reveal the presence of masses within the liver; most commonly, these are benign cysts.
Symptoms
The symptoms of abnormalities outside of the heart vary depending on the specific condition but often include:
- Chest Pain or Discomfort: Common in conditions like aortic aneurysm and pulmonary embolism.
- Shortness of Breath: Notable in pulmonary embolism and pericardial effusion.
- Swelling and Pain in Limbs: Associated with deep vein thrombosis and thoracic outlet syndrome.
- Dizziness or Fainting: Can occur due to reduced blood flow or cardiac output.
- Coughing or Wheezing: Especially in pulmonary conditions like embolism.
Causes
The causes of extracardiac abnormalities can be diverse:
- Genetic Factors: Conditions like coarctation of the aorta are often congenital, resulting from developmental issues during foetal growth.
- Lifestyle Factors: Smoking, high blood pressure, and high cholesterol can contribute to conditions like aortic aneurysms.
- Infections: Certain infections can lead to pericardial effusion.
- Trauma: Traumatic injuries can cause conditions like thoracic outlet syndrome or aortic dissection.
- Blood Clotting Disorders: These can lead to conditions such as deep vein thrombosis and pulmonary embolism.
- Inflammatory Diseases: Conditions like pericarditis can cause fluid accumulation around the heart.
Treatments
Treatment for abnormalities outside of the heart varies based on the specific condition, its severity, and the overall health of the patient. Here are some common treatments:
- Medications:
- Anticoagulants: Used to treat and prevent blood clots in conditions like pulmonary embolism and deep vein thrombosis.
- Anti-inflammatory Drugs: To reduce inflammation in conditions like pericarditis.
- Blood Pressure Medications: To manage conditions like aortic aneurysms and coarctation of the aorta.
- Surgical Interventions:
- Aortic Aneurysm Repair: Surgery to repair or replace the affected section of the aorta.
- Thrombectomy: Surgical removal of a blood clot, used in severe cases of pulmonary embolism.
- Pericardial Window or Pericardiocentesis: Procedures to remove excess fluid in cases of pericardial effusion.
- Surgical Decompression: For thoracic outlet syndrome, to relieve pressure on blood vessels or nerves.
- Minimally Invasive Procedures:
- Endovascular Stent Grafting: Used to treat aortic aneurysms by inserting a stent to support the weakened artery.
- Catheter-Based Thrombolysis: A technique to dissolve blood clots in the lungs or legs.
- Lifestyle Modifications:
- Diet and Exercise: To manage risk factors like hypertension and high cholesterol.
- Smoking Cessation: Reduces the risk of aneurysms and other vascular conditions.
The role of heart scans in identifying issues
Heart scans play a crucial role in diagnosing abnormalities outside of the heart, with advanced imaging techniques also providing detailed information about the cardiovascular system and surrounding structures, enabling accurate diagnosis and effective treatment planning. Key diagnostics include:
- Echocardiogram: Uses ultrasound to create detailed images of the heart, pericardium, and major blood vessels.
- Computed Tomography (CT) Scan: Provides detailed cross-sectional images of the chest and is particularly useful in detecting aortic aneurysms, pulmonary emboli, and other vascular abnormalities.
- Magnetic Resonance Imaging (MRI): Offers the most comprehensive assessment of soft tissues, making it valuable for diagnosing complex conditions like pericardial disease.
- Angiography: Involves injecting a contrast dye into the blood vessels to visualise blood flow and identify blockages or structural abnormalities in the arteries, essential for diagnosing and planning treatments for conditions like coarctation of the aorta.
The importance of trusting a professional Cardiac Clinic
Given the complexity and potential severity of abnormalities outside of the heart, it is crucial to seek care from a specialised cardiac clinic. Professional cardiac clinics offer several advantages:
- Expertise: Cardiologists and vascular specialists are trained to diagnose and treat an extensive range of cardiovascular and extracardiac conditions, ensuring patients receive the most accurate diagnosis and effective treatment plans.
- Advanced Technology: Professional cardiac clinics are equipped with state-of-the-art diagnostic tools and treatment technologies, such as advanced imaging systems and minimally invasive surgical equipment.
- Comprehensive Care: These clinics provide a multidisciplinary approach, bringing together cardiologists, vascular surgeons, radiologists, and other specialists to offer comprehensive care tailored to each patient's needs.
- Ongoing Monitoring: Regular follow-ups and monitoring are crucial for managing chronic conditions and preventing complications. Professional clinics ensure that patients receive consistent care and timely interventions when necessary.
- Patient Education: Educating patients about their condition, treatment options, and lifestyle modifications is a key aspect of care in professional cardiac clinics. Informed patients are better equipped to manage their health and adhere to treatment plans.
For more information on our services, contact our helpful and friendly team today, or alternatively, you can book an appointment at one of our specialist clinics online now.
Conclusion
Abnormalities outside of the heart, or extracardiac abnormalities, encompass a wide range of conditions that can significantly impact cardiovascular health. These conditions, such as aortic aneurysms, pulmonary embolisms, and pericardial effusion, vary in severity and require prompt and accurate diagnosis. Symptoms can include chest pain, shortness of breath, and swelling, and their causes range from genetic factors and infections to lifestyle choices and trauma.
Treatment options for extracardiac abnormalities include medications, surgical interventions, minimally invasive procedures, and lifestyle modifications.
Heart scans play a vital role in diagnosing these conditions, providing detailed images that guide effective treatment planning. Given the complexity of these conditions, trusting a professional cardiac clinic is essential. These clinics offer the expertise, advanced technology, comprehensive care, ongoing monitoring, and patient education needed to manage and treat extracardiac abnormalities effectively.
By seeking care from specialised professionals, patients can ensure the best possible outcomes for their cardiovascular health.
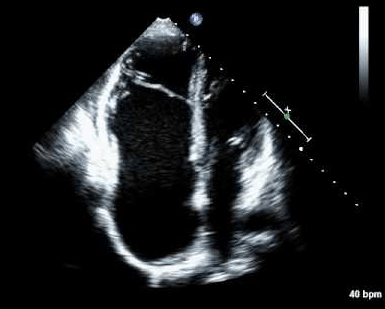
Significant congenital heart abnormalities are usually identified in childhood, but there is a possibility your scan may identify a structural anomaly that you were born with, such as a hole in the heart. This will need referral on to a Congenital Heart Disease specialist for further investigation.
What is Congenital Heart Disease?
Congenital heart disease (CHD) refers to a range of structural abnormalities of the heart that are present at birth. These defects can affect the heart's walls, valves, or blood vessels and impact how blood flows through the heart and to the rest of the body.
CHD is the most common type of birth defect, occurring in around 1 in 100 live births globally. The severity of CHD can vary greatly, from simple conditions that cause no symptoms to complex issues that require immediate medical intervention.
How serious is Congenital Heart Disease? & Are there different types?
The seriousness of congenital heart disease varies widely, as while some defects are minor and may resolve independently or require minimal treatment, others are more severe and can be life-threatening.
CHD is broadly categorised into critical and non-critical forms:
- Critical Congenital Heart Disease: This term refers to the most serious types of CHD that typically require surgery or other interventions within the first year of life. Examples include Hypoplastic Left Heart Syndrome, Transposition of the Great Arteries, and Tetralogy of Fallot. These conditions can severely impact the oxygenation of blood and overall heart function.
- Non-Critical Congenital Heart Disease: These defects are less severe and might not require immediate intervention. The common types include Atrial Septal Defect (ASD), Ventricular Septal Defect (VSD), and Patent Ductus Arteriosus (PDA). Although these conditions might not be immediately life-threatening, they can still cause significant health issues and often require medical attention.
Symptoms of CHD
Congenital heart disease symptoms can vary based on the specific type and severity of the defect. In some cases, symptoms may be present at birth, whilst in others, they might not appear until later in life.
Common symptoms include:
- Cyanosis: A bluish tint to the skin, lips, and fingernails due to low oxygen levels in the blood.
- Shortness of Breath: Particularly during feeding or physical activity in infants and children.
- Poor Feeding and Growth: Infants may struggle to feed properly and gain weight.
- Heart Murmurs: Unusual sounds heard during a heartbeat, indicating abnormal blood flow through the heart.
- Fatigue: General weakness and tiredness, especially during exertion.
- Swelling: In the legs, abdomen, or areas around the eyes due to fluid retention.
The causes of Congenital Heart Disease
Understanding what causes congenital heart disease involves examining both genetic and environmental factors, and whilst the exact causes of many CHD cases aren't fully understood, several risk factors have been identified:
- Genetic Factors: Genetic mutations and chromosomal abnormalities can increase the risk of CHD. Conditions like Down syndrome are associated with a higher incidence of heart defects. A family history of CHD also increases the likelihood of its occurrence.
- Environmental Factors: Maternal health and environmental exposures during pregnancy play a significant role. Factors such as maternal diabetes, infections (e.g., rubella), exposure to certain medications, alcohol, and smoking during pregnancy are known to elevate the risk of CHD.
- Multifactorial Inheritance: Often, CHD results from a combination of genetic predispositions and environmental influences. This multifactorial nature makes pinpointing a single cause challenging in many cases.
How is it diagnosed?
Early and accurate diagnosis of congenital heart disease is crucial for effective treatment, with the diagnostic process typically involving several steps and various techniques:
- Prenatal Screening:
- Ultrasound: Routine prenatal ultrasounds can sometimes detect heart defects before birth.
- Foetal Echocardiography: A specialised ultrasound that provides a detailed view of the foetal heart's structure and function, often used if there is a family history of CHD or other risk factors.
- Postnatal Diagnosis:
- Physical Examination: Doctors may detect heart murmurs or other signs during a routine check-up.
- Echocardiogram: This test uses sound waves to create detailed images of the heart, allowing doctors to see the structure and function of the heart in detail.
- Electrocardiogram (ECG): Measures the electrical activity of the heart to identify abnormalities.
- Chest X-ray: Helps visualise the heart's size and shape.
- Pulse Oximetry: Measures the oxygen level in the blood, which can indicate heart problems.
- Advanced Imaging and Tests:
- MRI and CT Scans: Provide detailed images, useful in diagnosing complex defects.
- Cardiac Catheterisation: Involves inserting a catheter into the heart to measure pressures, take blood samples, and sometimes treat defects.
Treatment for Congenital Heart Disease
The treatment for congenital heart disease depends on the type and severity of the defect, with options ranging from simple monitoring to complex surgical procedures:
- Medical Management:
- Medications: Diuretics, ACE inhibitors, or beta-blockers can help manage symptoms and improve heart function.
- Regular Monitoring: Regular follow-up appointments are essential to monitor heart function and growth.
- Surgical Treatment:
- Open-Heart Surgery: Required to repair or replace defective heart structures. Procedures may involve patching holes, repairing valves, or reconstructing blood vessels.
- Heart Transplant: In cases where the heart is severely damaged and other treatments are not viable, a heart transplant may be necessary.
- Catheter-Based Procedures:
- Balloon Angioplasty: Used to open narrowed blood vessels.
- Device Closure: Involves inserting devices via catheter to close holes in the heart.
- Hybrid Procedures: Combine surgery and catheter-based interventions for complex cases, providing a less invasive option with quicker recovery times.
The role of heart scans in identifying Congenital Heart Disease
Heart scans play a pivotal role in diagnosing and managing congenital heart disease. They provide detailed information about the heart's structure and function, which is crucial for accurate diagnosis and treatment planning.
- Echocardiograms: The most common and essential heart scan used in diagnosing CHD. It provides real-time images of the heart, allowing Doctors to see abnormalities in structure and function.
- Foetal Echocardiography: Conducted during pregnancy, it helps in early detection and planning for interventions that might be needed immediately after birth.
- MRI and CT Scans: Offer detailed cross-sectional images of the heart and surrounding blood vessels. These scans are particularly useful for complex cases where precise anatomical details are needed for surgical planning.
- Cardiac Catheterization: Though more invasive, this procedure provides detailed information about the heart’s internal structures and pressures and can also be therapeutic.
For more information on our services, contact our helpful and friendly team today, or alternatively, you can book an appointment at one of our specialist clinics online now.
In conclusion, congenital heart disease is a complex condition overall with a wide spectrum of severity and manifestations. Early diagnosis through advanced imaging techniques, combined with tailored treatment plans, can significantly improve outcomes for individuals with CHD. Ongoing research and medical advancements continue to enhance the quality of life for those living with congenital heart disease.
Cardiac masses, excluding those involving the heart valves, encompass a range of abnormalities such as tumours and thrombi that can form within the heart chambers or on the heart’s walls. These masses can interfere with normal heart function, leading to serious health complications if not properly diagnosed and treated.
This page covers the nature of these masses, including atrial myxomas and thrombi, their seriousness, symptoms, treatments, and the crucial role of heart scans in identifying these issues. Additionally, it emphasises the importance of seeking care from a professional cardiac clinic.
What are Atrial Myxomas?
Atrial myxomas are the most common type of primary heart tumours, with these non-cancerous growths typically arising from the left atrium but can also develop in the right atrium.
Atrial myxomas are composed of gelatinous material and are attached to the endocardium, the inner lining of the heart, often by a stalk. Despite being benign, their location within the heart can lead to significant complications.
How serious are Atrial Myxomas? & Are there different types?
Atrial myxomas are serious due to their potential to obstruct blood flow, cause embolism, and interfere with heart valves. They can vary in size and location, influencing the severity of their impact on heart function. While all atrial myxomas are benign, their seriousness lies in the mechanical and embolic complications they can cause.
What are the symptoms of Atrial Myxomas?
Atrial myxoma symptoms can vary widely, depending on the size, location, and mobility of the tumour.
Common symptoms include:
- Shortness of Breath: Due to obstruction of blood flow within the heart.
- Chest Pain: Caused by reduced blood flow to the heart muscle.
- Palpitations: Irregular heartbeats due to disrupted electrical activity.
- Dizziness or Fainting: Resulting from impaired blood flow to the brain.
- Embolic Events: Stroke or transient ischemic attack (TIA) due to fragments of the tumour breaking off and travelling to the brain or other organs.
- Systemic Symptoms: Fever, weight loss, and fatigue can also occur due to the tumour's presence.
How are they treated?
Atrial myxoma treatment primarily involves surgical removal of the tumour, with a procedure known as a myomectomy, which is typically performed via open-heart surgery. Successful removal usually leads to a complete cure, with a low risk of recurrence.Post-surgery, patients often require follow-up echocardiograms to monitor for any potential recurrence.
What is a Thrombus?
A thrombus is a blood clot that forms within a blood vessel or the heart. In the context of the heart, thrombi can form in any chamber but are particularly concerning when they develop in the left ventricle (LV thrombus) or atria. Unlike atrial myxomas, thrombi are not tumours but clotted blood that can obstruct blood flow or dislodge and travel to other parts of the body, causing embolic events.
How serious are Thrombi? & Are there different types?
Thrombi in the heart are extremely serious due to their potential to cause life-threatening complications, such as strokes, myocardial infarction, or pulmonary embolism. There are different types of thrombi based on their location:
- LV Thrombus: Forms in the left ventricle, often after a heart attack, and poses a high risk of embolism, particularly stroke.
- Atrial Thrombus: Commonly associated with atrial fibrillation, which leads to turbulent blood flow and clot formation.
What are the symptoms?
The symptoms of a blood clot in the heart depend on its size, location, and whether it causes embolism. Typical symptoms include:
- Chest Pain: Due to impaired blood flow.
- Shortness of Breath: Resulting from reduced cardiac output.
- Palpitations: Irregular heart rhythms due to disrupted flow.
- Swelling in Legs or Abdomen: Indicative of heart failure.
- Neurological Symptoms: Sudden weakness, numbness, or speech difficulties if a clot embolizes to the brain.
How are Thrombi treated?
Treatment of a thrombus involves:
- Anticoagulant Medications: To prevent further clotting and to help dissolve existing clots - common drugs include warfarin, heparin, and newer anticoagulants like apixaban and rivaroxaban.
- Thrombolytic Therapy: Administration of clot-dissolving drugs in acute settings.
- Surgical Interventions: In severe cases, surgical clot removal might be necessary.
The role of heart scans in identifying Cardiac Masses
Heart scans play a crucial role in identifying cardiac masses, including atrial myxomas and thrombi. Advanced imaging techniques provide detailed visualisations of the heart’s structures, helping in accurate diagnosis and treatment planning:
- Echocardiogram: This ultrasound-based test is the primary tool for detecting atrial myxomas and thrombi, providing real-time images of the heart chambers, valves, and surrounding structures.
- CT and MRI Scans: These imaging techniques offer detailed cross-sectional images, helping to assess the size, location, and characteristics of cardiac masses.
- Transesophageal Echocardiography (TEE): This internal scan provides more detailed imaging of the heart, which is especially useful for detecting smaller or more obscure masses.
The importance of trusting a professional Cardiac Clinic
Given the complexity and potential severity of cardiac masses, it is essential to trust a professional cardiac clinic for diagnosis and treatment. Attending a professional cardiac clinic offers several benefits:
- Expertise: Specialised cardiologists and cardiac surgeons have the expertise to accurately diagnose and effectively treat cardiac masses.
- Advanced Technology: Access to state-of-the-art diagnostic and treatment technologies ensures accurate assessments and effective interventions.
- Comprehensive Care: Multidisciplinary teams provide holistic care, addressing all aspects of a patient’s health and ensuring continuity of care.
- Personalised Treatment Plans: Individualised care plans tailored to each patient’s specific needs and conditions ensure the best possible outcomes.
For more information on our services, contact our helpful and friendly team today, or alternatively, you can book an appointment at one of our specialist clinics online now.
Conclusion
In conclusion, non-valvular cardiac masses such as atrial myxomas and thrombi are significant health concerns that require timely diagnosis and intervention. Understanding the symptoms, risks, and treatment options for these conditions is crucial for effective management.
Heart scans play a vital role in identifying these masses, and seeking care from a professional cardiac clinic ensures that patients receive the highest standard of care, by trusting in specialised professionals, patients can achieve better health outcomes and mitigate the risks associated with these potentially life-threatening conditions.
Book Your Heart Scan Today